Escolar Documentos
Profissional Documentos
Cultura Documentos
Blood Group
Enviado por
nyangara0 notas0% acharam este documento útil (0 voto)
115 visualizações38 páginasKarl Landsteiner discovered the main human blood group systems in 1901 which paved the way for safe blood transfusions. He found that mixing blood from different individuals could cause clumping of red blood cells due to antibodies in the plasma reacting to antigens on red blood cells. There are over 20 blood group systems but the ABO and Rh systems are most important. A person's blood group depends on which antigens and antibodies they inherit from their parents. The ABO blood group is determined by genes on chromosome 9 which can be dominant or co-dominant.
Descrição original:
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoKarl Landsteiner discovered the main human blood group systems in 1901 which paved the way for safe blood transfusions. He found that mixing blood from different individuals could cause clumping of red blood cells due to antibodies in the plasma reacting to antigens on red blood cells. There are over 20 blood group systems but the ABO and Rh systems are most important. A person's blood group depends on which antigens and antibodies they inherit from their parents. The ABO blood group is determined by genes on chromosome 9 which can be dominant or co-dominant.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
115 visualizações38 páginasBlood Group
Enviado por
nyangaraKarl Landsteiner discovered the main human blood group systems in 1901 which paved the way for safe blood transfusions. He found that mixing blood from different individuals could cause clumping of red blood cells due to antibodies in the plasma reacting to antigens on red blood cells. There are over 20 blood group systems but the ABO and Rh systems are most important. A person's blood group depends on which antigens and antibodies they inherit from their parents. The ABO blood group is determined by genes on chromosome 9 which can be dominant or co-dominant.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 38
Co-dominance
Blood groups and Rhesus
factor
Dr.Nyangara Rajabu Mtilly, MD, Mmed
Student, IMTU
Glossary
Gene
Locus
Allele
Heterozygous
Homozygous
Phenotype
Genotype
Sex Chromosome
Autosomal Chromosome
Dominant Gene
Recessive Gene
Chromosomes
Chromosomes are made up of DNA
Make up genes
Code for proteins
Glossary
Heterozygous
2 identical chromosomes with DIFFERENT
Gene types i.e. Dominant & Recessive
Homozygous
2 identical chromosomes with the SAME
genes on each chromosome ie Dominant &
Dominant
Glossary
Locus
Location of a gene on a chromosome
Allele
Variation of a gene that produces an alternative
Phenotype
Phenotype
The result of expressing a gene ie Hair colour
Gene
A section of DNA made of bases that code for a
phenotype. ie eye colour
Glossary
Sex Linked Chromosome
Is either X or Y. Determines gender. Females
have XX, males have XY
Autosomal Chromosome
Pairs of chromosomes that have identical gene
location, and are the same in Male and
Females. Only the code within the gene varies.
Glossary
Dominant Gene
A strong gene that only needs one copy on one
chromosome to be expressed.
Recessive gene
Weak gene that needs a copy on each
autosomal chromosome (M&F), or on each
XX in women, or on the X in men, to be
expressed
The Blood Group Systems
Inheritance and Genetics
History of Blood Groups and Blood Transfusions
Experiments with blood transfusions
have been carried out for hundreds of
years. Many patients have died and it was
not until 1901, when the Austrian Karl
Landsteiner discovered human blood
groups, that blood transfusions became
safer.
He found that mixing blood from two
individuals can lead to blood clumping.
The clumped RBCs can crack and cause
toxic reactions. This can be fatal.
http://nobelprize.org/medicine/educational/landsteiner/readmore.html
Karl Landsteiner discovered that blood
clumping was an immunological reaction
which occurs when the receiver of a blood
transfusion has antibodies against the donor
blood cells.
Karl Landsteiner's work made it possible to
determine blood types and thus paved the
way for blood transfusions to be carried out
safely. For this discovery he was awarded the
Nobel Prize in Physiology or Medicine in
1930.
History of Blood Groups and Blood
Transfusions (Cont.)
What is blood made up of?
An adult human has about 46 liters of
blood circulating in the body.
Blood consists of several types of cells
floating around in a fluid called plasma.
The red blood cells (RBCs) contain
haemoglobin, a protein that binds oxygen.
RBCs transport oxygen to, and remove
carbon dioxide from the tissues.
The white blood cells fight infection.
The platelets help the blood to clot, if you
get a wound for example.
The plasma contains salts and various
kinds of proteins.
Blood Groups, Blood Typing and Blood
Transfusions
The discovery of blood groups
Experiments with blood transfusions, the transfer of blood or blood components into a person's blood
stream, have been carried out for hundreds of years. Many patients have died and it was not until
1901, when the Austrian Karl Landsteiner discovered human blood groups, that blood transfusions
became safer.
Mixing blood from two individuals can lead to blood clumping or agglutination. The clumped red cells
can crack and cause toxic reactions. This can have fatal consequences. Karl Landsteiner discovered
that blood clumping was an immunological reaction which occurs when the receiver of a blood
transfusion has antibodies against the donor blood cells.
Karl Landsteiner's work made it possible to determine blood types and thus paved the way for blood
transfusions to be carried out safely. For this discovery he was awarded the Nobel Prize in Physiology
or Medicine in 1930.
Blood group 0
If you belong to the blood group 0 (null), you have neither A or B antigens on the surface of your red
blood cells but you have both A and B antibodies in your blood plasma.
The differences in human blood are due to the
presence or absence of certain protein molecules
called antigens and antibodies.
The antigens are located on the surface of the
RBCs and the antibodies are in the blood
plasma.
Individuals have different types and
combinations of these molecules.
The blood group you belong to depends on
what you have inherited from your parents.
What are the different blood groups?
There are more than 20 genetically determined
blood group systems known today
The AB0 and Rhesus (Rh) systems are the
most important ones used for blood transfusions.
Not all blood groups are compatible with each
other. Mixing incompatible blood groups leads to
blood clumping or agglutination, which is
dangerous for individuals.
What are the different blood groups?
According to the ABO blood
typing system there are four
different kinds of blood types:
A, B, AB or O (null).
ABO blood grouping system
Blood group A
If you belong to the blood
group A, you have A
antigens on the surface of
your RBCs and B
antibodies in your blood
plasma.
Blood group B
If you belong to the blood
group B, you have B
antigens on the surface of
your RBCs and A
antibodies in your blood
plasma.
AB0 blood grouping system
Blood Groups, Blood Typing and
Blood Transfusions
The discovery of blood groups
Experiments with blood transfusions, the transfer of blood or blood components
into a person's blood stream, have been carried out for hundreds of years. Many
patients have died and it was not until 1901, when the Austrian Karl Landsteiner
discovered human blood groups, that blood transfusions became safer.
Mixing blood from two individuals can lead to blood clumping or agglutination.
The clumped red cells can crack and cause toxic reactions. This can have fatal
consequences. Karl Landsteiner discovered that blood clumping was an
immunological reaction which occurs when the receiver of a blood transfusion
has antibodies against the donor blood cells.
Karl Landsteiner's work made it possible to determine blood types and thus
paved the way for blood transfusions to be carried out safely. For this discovery
he was awarded the Nobel Prize in Physiology or Medicine in 1930.
What is blood made up of?
An adult human has about 46 liters of blood circulating in the body. Among
other things, blood transports oxygen to various parts of the body.
Blood consists of several types of cells floating around in a fluid called plasma.
The red blood cells contain hemoglobin, a protein that binds oxygen. Red
blood cells transport oxygen to, and remove carbon dioxide from, the body
tissues.
The white blood cells fight infection.
The platelets help the blood to clot, if you get a wound for example.
The plasma contains salts and various kinds of proteins.
What are the different blood groups?
The differences in human blood are due to the presence or absence of certain
protein molecules called antigens and antibodies. The antigens are located on
the surface of the red blood cells and the antibodies are in the blood plasma.
Individuals have different types and combinations of these molecules. The blood
group you belong to depends on what you have inherited from your parents.
There are more than 20 genetically determined blood group systems known
today, but the AB0 and Rh systems are the most important ones used for blood
transfusions. Not all blood groups are compatible with each other. Mixing
incompatible blood groups leads to blood clumping or agglutination, which is
dangerous or individuals.
Nobel Laureate Karl Landsteiner was involved in the discovery of both the AB0
and Rh blood groups.
AB0 blood grouping system
Blood group AB
If you belong to the blood group
AB, you have both A and B
antigens on the surface of your
RBCs and no A or B antibodies
at all in your blood plasma.
Blood group O
If you belong to the blood group O
(null), you have neither A or B
antigens on the surface of your RBCs
but you have both A and B antibodies
in your blood plasma.
The "A and "B" antigens are also produced
by some other plants and microorganisms.
Thus, individuals who do not recognize one or
more of these antigens as "self" will produce
antibodies against the plant or microbial
antigens.
These antibodies will also react with human
antigens of the same kind whether introduced
via a blood transfusion or a tissue graft.
Why do individuals produce antibodies to
antigens they do not have?
The ABO gene is autosomal (the gene is not on either sex
chromosomes)
The ABO gene locus is located on the chromosome 9.
Each person has two copies of genes coding for their ABO blood
group (one maternal and one paternal in origin)
A and B blood groups are dominant over the O blood group
A and B group genes are co-dominant
ABO inheritance and genetics
AUTOSOMAL
CHROMOSOME
Mustafa
Sara
one alleles from Mustafa and one
from Sara.
The alleles for Blood
group are in the same
place on the
chromosome 9. However
the genes have a
different code giving the
different blood group
A B
This meant that if a person inherited one A group gene and one
B group gene their red cells would possess both the A and B
blood group antigens.
These alleles were termed A ( which produced the A antigen ),
B (which produced the B antigen) and O (which was "non
functional"and produced no A or B antigen)
What do co-dominant genes mean?
Parent
Allele
A B O
A
B
O
Possible Blood group Genotypes
Parent
Allele
A B O
A AA AB AO
B AB BB BO
O AO BO OO
Possible Blood group Genotypes
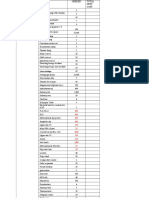
The ABO blood groups
The most important in assuring a safe blood transfusion.
The table shows the four ABO phenotypes ("blood groups") present
in the human population and the genotypes that give rise to them.
Blood
Group
Antigens
on RBCs
Antibodies in Serum Genotypes
A A Anti-B AA or AO
B B Anti-A BB or BO
AB A and B Neither AB
O Neither Anti-A and anti-B OO
Why group A blood must never be
given to a group B person?
Giving someone blood from the wrong ABO
group could be fatal.
The anti-A antibodies in group B attack group
A cells and vice versa.
Blood group O negative is a different story.
Well, it gets more complicated here, because there's
another antigen to be considered - the Rh antigen.
Some of us have it, some of us don't.
If it is present, the blood is RhD positive, if not it's RhD
negative.
So, for example, some people in group A will have it, and
will therefore be classed as A+ (or A positive).
While the ones that don't, are A- (or A negative).
And so it goes for groups B, AB and O.
The Rhesus (Rh) System
Rh antigens are transmembrane proteins with loops
exposed at the surface of red blood cells.
They appear to be used for the transport of carbon
dioxide and/or ammonia across the plasma membrane.
They are named for the rhesus monkey in which they
were first discovered.
RBCs that are "Rh positive" express the antigen
designated D.
85% of the population is RhD positive, the other 15%
of the population is running around with RhD negative
blood.
The Rhesus (Rh) System (Cont.)
Blood
Type
Genotype
Alleles
Produced
Rh positive
RR R
Rr R or r
Rh negative rr r
Rh Blood Group and Rh Incompatibility
A person with Rh- blood does not have Rh
antibodies naturally in the blood plasma
According to above
blood grouping systems,
you can belong to either
of following 8 blood
groups:
Do you know which blood group you
belong to?
A person with Rh- blood can develop Rh antibodies
in the blood plasma if he or she receives blood from a
person with Rh+ blood, whose Rh antigens can trigger
the production of Rh antibodies.
A person with Rh+ blood can receive blood from
a person with Rh- blood without any problems.
Why is an Rh incompatibility so dangerous
when ABO incompatibility is not during
pregnancy?
Most anti-A or anti-B antibodies are of the IgM
class (large molecules) and these do not cross the
placenta.
In fact, an Rh
/type O mother carrying an
Rh
+
/type A, B, or AB foetus is resistant to
sensitisation to the Rh antigen.
Her anti-A and anti-B antibodies destroy any foetal
cells that enter her blood before they can elicit anti-
Rh antibodies in her.
This phenomenon has led to an effective
preventive measure to avoid Rh sensitisation.
Shortly after each birth of an Rh
+
baby, the
mother is given an injection of anti-Rh
antibodies (or Rhogam).
These passively acquired antibodies destroy
any foetal cells that got into her circulation
before they can elicit an active immune
response in her.
Rh incompatibility during pregnancy (cont.)
The ABO Blood Group System
Laboratory Determination of the
ABO System
Several methods for testing the ABO group of an
individual exist. The most common method is:
Serology: This is a direct detection of the ABO
antigens. It is the main method used in blood
transfusion centres and hospital blood banks.
This form of testing involves two components:
a) Antibodies that are specific at detecting a
particular ABO antigen on RBCs.
b) Cells that are of a known ABO group that
are agglutinated by the naturally occurring
antibodies in the person's serum.
Illustration of the forward and reverse
grouping reaction patterns of the ABO
groups using a blood group tile
http://www.bh.rmit.edu.au/mls/subjects/abo/resources/genetics1.htm
When RBCs carrying one or both antigens are exposed to the
corresponding antibodies, they agglutinate; that is, clump
together. People usually have antibodies against those red cell
antigens that they lack.
Human RBC before (left) and after (right) adding serum
containing anti-A antibodies. The agglutination reaction
reveals the presence of the A antigen on the surface of the
cells.
http://users.rcn.com/jkimball.ma.ultranet
/BiologyPages/B/BloodGroups.html
People with blood group O
are called "universal
donors" and people with
blood group AB are called
"universal receivers."
Blood transfusions who can
receive blood from
whom?
Blood
Group
Antigens Antibodies Can give
blood to
Can
receive
blood from
AB
A
B
O
Blood
Group
Antigens Antibodies Can give
blood to
Can
receive
blood from
AB A and B None AB AB, A, B, O
A A B A and AB A and O
B B A B and AB B and O
O None A and B AB, A, B, O O
Você também pode gostar
- Working of Blood BanksDocumento146 páginasWorking of Blood BanksRupali Vaiti100% (1)
- Blood Groups: HAP Unit 5thDocumento31 páginasBlood Groups: HAP Unit 5thSNEHASIS POLLEYAinda não há avaliações
- Connective TissuesDocumento5 páginasConnective Tissuesraphael100% (1)
- Blood TypingDocumento8 páginasBlood TypingAbby Umali-HernandezAinda não há avaliações
- Uterine FibroidsDocumento30 páginasUterine Fibroidsbabudocs1Ainda não há avaliações
- Uterine FibroidsDocumento30 páginasUterine Fibroidsbabudocs1Ainda não há avaliações
- Sex Determination and InheritanceDocumento61 páginasSex Determination and Inheritancedaniel dennis encarta100% (1)
- The Blood Group Systems: Inheritance and GeneticsDocumento34 páginasThe Blood Group Systems: Inheritance and GeneticsP Vinod Kumar100% (1)
- Blood TypingDocumento34 páginasBlood Typingaurezea100% (1)
- Michael Chinery-Insects of Britain and Western Europe-Revised 2007 EditionDocumento324 páginasMichael Chinery-Insects of Britain and Western Europe-Revised 2007 EditionDIPOLMEDIA100% (6)
- Co-Dominance Blood Groups and Rhesus Factor: DR - Mohammed Iqbal Musani, MDDocumento38 páginasCo-Dominance Blood Groups and Rhesus Factor: DR - Mohammed Iqbal Musani, MDisasai52Ainda não há avaliações
- Blood Groups, Blood Transfusion & Rhesus FactorDocumento38 páginasBlood Groups, Blood Transfusion & Rhesus FactorUzma KhanAinda não há avaliações
- 11 - Forensic SerologyDocumento67 páginas11 - Forensic SerologyNurul HaziqahAinda não há avaliações
- Blood Test Lab ReportDocumento6 páginasBlood Test Lab Reportapi-282911691100% (1)
- ABO Blood Group SystemDocumento3 páginasABO Blood Group SystemSawan ShahAinda não há avaliações
- Book Tangent Worlds S v2Documento167 páginasBook Tangent Worlds S v2Данил КеллерAinda não há avaliações
- Biology Decade by Decade Twentieth Century ScienceDocumento369 páginasBiology Decade by Decade Twentieth Century SciencePutri MarlisaAinda não há avaliações
- 4 - Cell JunctionsDocumento25 páginas4 - Cell JunctionsKhdhir M. Salem100% (1)
- 1.blood GroupDocumento38 páginas1.blood GroupteraraAinda não há avaliações
- Wound Healing and RepairDocumento54 páginasWound Healing and RepairnyangaraAinda não há avaliações
- Chapter7 B and T Cell Activation (1) ImmunologyDocumento21 páginasChapter7 B and T Cell Activation (1) ImmunologyIka BakarAinda não há avaliações
- EthologyDocumento31 páginasEthologyKelompok 5 Profdok 17100% (2)
- Allen RZCDocumento67 páginasAllen RZC100T DweePAinda não há avaliações
- Serologi ForensikDocumento65 páginasSerologi ForensikbayuAinda não há avaliações
- Apologia Biology Vocabulary Crossword Module 11Documento3 páginasApologia Biology Vocabulary Crossword Module 11Shairuz Caesar Briones DugayAinda não há avaliações
- Trial of ScarDocumento12 páginasTrial of Scarnyangara50% (2)
- Blood Relations: Transfusion and the Making of Human GeneticsNo EverandBlood Relations: Transfusion and the Making of Human GeneticsAinda não há avaliações
- Blood GroupingDocumento3 páginasBlood GroupingShanmuga Priya Shanmuga PriyaAinda não há avaliações
- Blood Groups: Blood Is A Specialized Bodily Fluid That Delivers Necessary Substances To The Body'sDocumento11 páginasBlood Groups: Blood Is A Specialized Bodily Fluid That Delivers Necessary Substances To The Body'sayyappan6031Ainda não há avaliações
- Blood Grouping Experiment (Theory) - Immunology Virtual Lab I - Biotechnology and Biomedical Engineering - Amrita Vishwa Vidyapeetham Virtual LabDocumento5 páginasBlood Grouping Experiment (Theory) - Immunology Virtual Lab I - Biotechnology and Biomedical Engineering - Amrita Vishwa Vidyapeetham Virtual LabUzma KhanAinda não há avaliações
- Blood Groups: HAP Unit 5thDocumento31 páginasBlood Groups: HAP Unit 5thC RonaldoAinda não há avaliações
- LAB 3 - Blood TypingDocumento8 páginasLAB 3 - Blood TypingCodespher3Ainda não há avaliações
- Blood Groups, Blood Typing and Blood TransfusionsDocumento27 páginasBlood Groups, Blood Typing and Blood TransfusionsvishalkumarmorwalAinda não há avaliações
- Index: S.No Content Page NoDocumento11 páginasIndex: S.No Content Page NoAufin SmartAinda não há avaliações
- ABO Blood Grouping Cbsebiology4uDocumento15 páginasABO Blood Grouping Cbsebiology4uanandbhanwalkar111Ainda não há avaliações
- Blood DopingDocumento10 páginasBlood DopingAjay Pal NattAinda não há avaliações
- Blood Group System - EssayDocumento9 páginasBlood Group System - EssayMarleth100% (1)
- Blood GroupsDocumento5 páginasBlood GroupsMalik IrfanAinda não há avaliações
- Blood GroupDocumento17 páginasBlood GroupAvnish BhasinAinda não há avaliações
- Blood 2 FunctionsDocumento7 páginasBlood 2 FunctionsLukas IspasAinda não há avaliações
- 2 4 6 Neuro 1 Sistem Penggolongan Darah 3 Maret 2013Documento91 páginas2 4 6 Neuro 1 Sistem Penggolongan Darah 3 Maret 2013sari antiAinda não há avaliações
- Blood Grouping 12thDocumento17 páginasBlood Grouping 12thPranjal SharmaAinda não há avaliações
- Forensic Serology: Courtesy of C. FanningDocumento42 páginasForensic Serology: Courtesy of C. FanningSadiqa IqbalAinda não há avaliações
- ABO Blood Grouping Cbsebiology4uDocumento14 páginasABO Blood Grouping Cbsebiology4uRahit BiswasAinda não há avaliações
- ABO Blood Grouping Cbsebiology4uDocumento10 páginasABO Blood Grouping Cbsebiology4usorojsahu85Ainda não há avaliações
- Blood TypesDocumento7 páginasBlood Typesnma tofiqAinda não há avaliações
- Describe The Components of Blood?Documento64 páginasDescribe The Components of Blood?Ankur AthuniAinda não há avaliações
- Blood Group MLDDocumento5 páginasBlood Group MLDHarsheen KaurAinda não há avaliações
- Blood GroupsDocumento26 páginasBlood GroupsBhat MaryamAinda não há avaliações
- Information of Blood Group and Its ImportanceDocumento1 páginaInformation of Blood Group and Its ImportancesawlaninAinda não há avaliações
- BloodtransfusieDocumento79 páginasBloodtransfusieGod RaAinda não há avaliações
- ABO Blood GroupDocumento12 páginasABO Blood GroupGhost AnkanAinda não há avaliações
- PollinationDocumento16 páginasPollinationR.KABILANAinda não há avaliações
- Abo Blood Group SystemDocumento17 páginasAbo Blood Group SystemCSC LanjipadarAinda não há avaliações
- MLS 201 Lecture Note - Introduction To BGSDocumento7 páginasMLS 201 Lecture Note - Introduction To BGSBarry AllenAinda não há avaliações
- Abo Group.Documento33 páginasAbo Group.R.KABILANAinda não há avaliações
- Historical Background: William Harvey CirculationDocumento9 páginasHistorical Background: William Harvey Circulationmeku mekuAinda não há avaliações
- LECTURE Blood GroupingDocumento31 páginasLECTURE Blood Groupingjaveria choudharyAinda não há avaliações
- Blood Basics - Unit 5Documento10 páginasBlood Basics - Unit 5api-292042538Ainda não há avaliações
- Bloodbasics 1Documento10 páginasBloodbasics 1api-203306348Ainda não há avaliações
- ABO Blood Group SystemDocumento14 páginasABO Blood Group SystemsankaiyahAinda não há avaliações
- Blood Groups and Blood Transfusion BioDocumento23 páginasBlood Groups and Blood Transfusion BiowhyyoucareAinda não há avaliações
- Bio ProjectDocumento10 páginasBio Projectshwetanshu2109Ainda não há avaliações
- Information About BloodDocumento4 páginasInformation About BloodCalvin ChinAinda não há avaliações
- Blood TypingDocumento6 páginasBlood TypingmaniiiiiiiiAinda não há avaliações
- Blood TypesDocumento1 páginaBlood TypesTevae ShoelsAinda não há avaliações
- GST201-Study Session 7Documento16 páginasGST201-Study Session 7Elujulo OyinkansolaAinda não há avaliações
- Blood Typing Research PaperDocumento2 páginasBlood Typing Research Paperapi-273800330Ainda não há avaliações
- Blood BasicsDocumento10 páginasBlood BasicsProcess EngineerAinda não há avaliações
- Biology Investigatory Blood GroupDocumento13 páginasBiology Investigatory Blood Groupanonymous user 345Ainda não há avaliações
- Safe Blood: Purifying the Nations Blood Supply in the Age of ANo EverandSafe Blood: Purifying the Nations Blood Supply in the Age of AAinda não há avaliações
- Pre and Post TestDocumento11 páginasPre and Post TestnyangaraAinda não há avaliações
- Chop Q2-3Documento1 páginaChop Q2-3nyangaraAinda não há avaliações
- Partogram Case StudiesDocumento6 páginasPartogram Case StudiesnyangaraAinda não há avaliações
- Up Dated Respectiful Maternity Care (RMC)Documento21 páginasUp Dated Respectiful Maternity Care (RMC)nyangaraAinda não há avaliações
- 29.06.2018 MD 4 ExamDocumento8 páginas29.06.2018 MD 4 ExamnyangaraAinda não há avaliações
- Partogram Case StudiesDocumento6 páginasPartogram Case StudiesnyangaraAinda não há avaliações
- Applied Anatomy Edited 25 08 07-1Documento45 páginasApplied Anatomy Edited 25 08 07-1nyangaraAinda não há avaliações
- CGDDocumento43 páginasCGDnyangaraAinda não há avaliações
- Association and CausationDocumento16 páginasAssociation and CausationnyangaraAinda não há avaliações
- AMENORRHOEADocumento35 páginasAMENORRHOEAnyangaraAinda não há avaliações
- The Cell and Its Organelles PPDocumento94 páginasThe Cell and Its Organelles PPnyangaraAinda não há avaliações
- Obstetric FistulaeDocumento24 páginasObstetric FistulaenyangaraAinda não há avaliações
- Bus 5011 - Marketing ResearchDocumento62 páginasBus 5011 - Marketing ResearchnyangaraAinda não há avaliações
- Martenal Mortality 11.jan 2012Documento42 páginasMartenal Mortality 11.jan 2012nyangaraAinda não há avaliações
- Menopause Semester 6 (IMTU)Documento37 páginasMenopause Semester 6 (IMTU)nyangaraAinda não há avaliações
- Benign Disease of The UterusDocumento27 páginasBenign Disease of The UterusnyangaraAinda não há avaliações
- ShockDocumento7 páginasShockapi-3822433100% (2)
- Screening of DiseasesDocumento15 páginasScreening of Diseasesnyangara100% (1)
- PPH by Dr. Rajabu Nyangara MtillyDocumento38 páginasPPH by Dr. Rajabu Nyangara MtillynyangaraAinda não há avaliações
- Natural History of DiseaseDocumento34 páginasNatural History of Diseasenyangara100% (1)
- What Is InflammationDocumento17 páginasWhat Is InflammationnyangaraAinda não há avaliações
- Sexually Transmmited Diseases: Presenter: Nyangara Rajabu Facilitator: Isaac U. MDocumento31 páginasSexually Transmmited Diseases: Presenter: Nyangara Rajabu Facilitator: Isaac U. MnyangaraAinda não há avaliações
- Underwood: Chapter 6: Thrombosis, Embolism and InfarctionDocumento12 páginasUnderwood: Chapter 6: Thrombosis, Embolism and InfarctionnyangaraAinda não há avaliações
- Underwood: Chapter 6: Thrombosis, Embolism and InfarctionDocumento12 páginasUnderwood: Chapter 6: Thrombosis, Embolism and InfarctionnyangaraAinda não há avaliações
- Edward JennerDocumento3 páginasEdward JennernyangaraAinda não há avaliações
- Lifecycle of A House FlyDocumento4 páginasLifecycle of A House FlyAllison Nadine MarchandAinda não há avaliações
- Elementary Reading Comprehension Test 01Documento3 páginasElementary Reading Comprehension Test 01Amairani ChávezAinda não há avaliações
- What Is Cell Theory Science Presentation in Blue Yellow Hand Drawn StyleDocumento12 páginasWhat Is Cell Theory Science Presentation in Blue Yellow Hand Drawn StyleCarsten HerreraAinda não há avaliações
- Animals: General Characteristics of AnimalsDocumento4 páginasAnimals: General Characteristics of AnimalsAimheeAinda não há avaliações
- Animal Kingdom Non ChordataDocumento26 páginasAnimal Kingdom Non ChordataRaichal P BijuAinda não há avaliações
- Humans Body Systems QuestionsDocumento2 páginasHumans Body Systems QuestionsMichael PlexousakisAinda não há avaliações
- HSEB Question Collection Series - Biology 2069 XI - HSEB NOTESDocumento1 páginaHSEB Question Collection Series - Biology 2069 XI - HSEB NOTESHSEB Notes25% (4)
- Biology Grade 7 - Ujian Mid Semester 2 (Mis)Documento3 páginasBiology Grade 7 - Ujian Mid Semester 2 (Mis)Maggie Y. MontungAinda não há avaliações
- The Living World - Speed Practice Sheet - Arjuna NEET 2.0 2024Documento5 páginasThe Living World - Speed Practice Sheet - Arjuna NEET 2.0 2024hasanbuilders676Ainda não há avaliações
- Department of Education: Science IvDocumento2 páginasDepartment of Education: Science IvCristita Macaranas Vigo100% (1)
- FrogDocumento28 páginasFrogSujay RankAinda não há avaliações
- Human Embryonic Development From Peri-Implantation To GastrulationDocumento12 páginasHuman Embryonic Development From Peri-Implantation To GastrulationscribdarnabAinda não há avaliações
- Book Edcoll 9789004261051 B9789004261051-S017-PreviewDocumento2 páginasBook Edcoll 9789004261051 B9789004261051-S017-PreviewRommel AnastacioAinda não há avaliações
- Primary Cell Culture 2013 020914Documento40 páginasPrimary Cell Culture 2013 020914nurhanamjAinda não há avaliações
- Cells and OrganismDocumento29 páginasCells and OrganismMohammed FazilAinda não há avaliações
- Name:Muhammad Nukman Thaqif Bin Yusri Matric No:D61316Documento51 páginasName:Muhammad Nukman Thaqif Bin Yusri Matric No:D61316MUHAMMAD AFHAM SADIQ BIN YUSRI Moe100% (1)
- Except: - Best of LuckDocumento1 páginaExcept: - Best of LuckAnisa Al FitriAinda não há avaliações
- Grade 3 2nd Quarter Unit 4 Lesson 1 Body Parts of Animals and Their FunctionsDocumento28 páginasGrade 3 2nd Quarter Unit 4 Lesson 1 Body Parts of Animals and Their FunctionsRaul Rivera SantosAinda não há avaliações
- Form 4 Science Chapter 2Documento13 páginasForm 4 Science Chapter 2Cheah Foo Kit50% (2)
- CellsDocumento7 páginasCellsJeremiah CromartieAinda não há avaliações