Escolar Documentos
Profissional Documentos
Cultura Documentos
Asthma by DR Sarma
Enviado por
Surbhi JoshiTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Asthma by DR Sarma
Enviado por
Surbhi JoshiDireitos autorais:
Formatos disponíveis
Dr.
Sarma@works
1
LIFE TIME HAPPINESS
Dr.Sarma@works
2
When you can't breathe,
nothing else matters
3
Dr.Sarma@works
CD format of todays presentation is ready
1. Asthma, COPD and Basics of Spirometry
In addition it, also contains
2. ECG workshop presented earlier
3. Guidelines on Hypertension treatment
This can be used in Computer & DVD player
Important Announcement
Dr.Sarma@works
4
1. ACCP www.chestnet.org
2. ATS www.thoracic.org
3. BTS www.brit-thoracic.org.uk
4. COPD profess. www.copdprofessional.com
5. GOLD www.goldcopd.com
6. NICE www.nice.uk.org
7. Chest Net www.chestnet.net
8. CDC www.cdc.nih.gov
9. NAEPP www.naepp.nhlbi.org
10.COPD Rapid series by ELSEVIER
COPD and Asthma Resources
Dr.Sarma@works
5
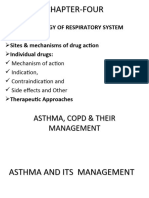
CHRONIC LUNG DISEASES
Pulmonary Tuberculosis
Restrictive lung diseases
Suppurative lung disease
Obstructive lung diseases
Bronchial Asthma
Chronic bronchitis
Emphysema and
Their differentiations
Dr.Sarma@works
6
AN OVERVIEW - GINA
MANAGEMENT GUIDE LINES
Dr. Sarma.R.V.S.N., M.D., M.Sc
(Canada)
Consultant Physician and chest specialist
# 5, Jayanagar, Tiruvallur 602 001
+ 91 9894- 60593, (4116) 260593
ASTHMA
Dr.Sarma@works
7
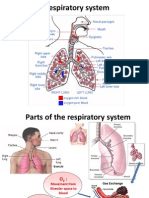
WHAT IS ASTHMA ?
Primarily it is an allergic inflam-
matory disorder of the airways
Infiltration of mast cells, eosinophils
and lymphocytes
Secondary broncho-constriction
Airway hyper-responsiveness
Recurrent episodes of wheezing,
coughing and shortness of breath
Airflow limitation is variable and
often reversible and wide spread
Dr.Sarma@works
8
BURDEN OF ILLNESS
15- 20 million asthmatics in India.
A recent study conducted in Delhi
established asthma prevalence to be
12% in school children.
Significant cause of school/work absence.
Health care expenditures very high.
Morbidity and mortality are on the rise.
Dr.Sarma@works
9
THE HUGE GAP
Patients are not detected
Do not seek medical attention
No access to health service
Stigma associated with the label
Broken marriages, alliances
Missed diagnosis (bronchitis, LRTI)
MECHANISM OF ASTHMA
INFLAMMATION
Risk Factors (for development of asthma)
Airway
Hyper responsiveness
Airflow
Limitation
Symptoms- (shortness of
breath, cough, wheeze)
Risk Factors
(for exacerbations)
Dr.Sarma@works
11
ASTHMA : PATHOLOGY
Dr.Sarma@works
12
RISK FACTORS FOR ASTHMA
Predisposing Factors
Atopy ( IgE)
Causal Factors
Indoor Allergens
Domestic mites
Animal Allergens
Cockroach Allergens
Fungi moulds
Outdoor Allergens
Pollens
Fungi, RSV
Occupational
Sensitizers
Contributing Factors
Respiratory infections
Small size at birth
Diet
Air pollution
Outdoor pollutants
Indoor pollutants
Smoking
Passive Smoking
Active Smoking
Dr.Sarma@works
13
HOUSE DUST MITE
Use bedding encasements
Wash bed linens weekly
Avoid down fillings
Limit stuffed toys to those
that can be washed
Reduce humidity level
Dr.Sarma@works
14
COCKROACHES
Remove as many
water and food
sources as
possible to avoid
cockroaches.
Dr.Sarma@works
15
PETS
People allergic to pets should not
have them in the house.
At a minimum, do not allow pets in
the bedroom.
Dr.Sarma@works
16
MOLDS - FUNGUS
Eliminating mold may help control asthma exacerbations.
Dr.Sarma@works
17
History and patterns of symptoms
Physical examination
Measurements of lung function
Peak flow meter
Spirometry
DIAGNOSIS OF ASTHMA
Dr.Sarma@works
18
PATIENT HISTORY
Has the patient had an attack or recurrent
episodes of wheezing?
Does the patient have a troublesome cough,
worse particularly at night, or on awakening?
Does the patient cough after physical activity
(eg. Playing)?
Does the patient have breathing problems
during a particular season (or change of
season)?
Dr.Sarma@works
19
MAIN SYMPTOM CLUES
Do the patients colds go to the chest or
take more than 10 days to resolve?
Does the patient use any medication ?
(e.g. bronchodilator) when symptoms
occur ? - Is there a (relief) response?
If the patient answers YES to any of the
above questions, suspect asthma.
Remember, the commonest cause of
persistent cough is asthma
Dr.Sarma@works
20
PHYSICAL EXAM
Wheeze -
Usually heard without a stethoscope
Dyspnoea -
Rhonchi heard with a stethoscope
Use of accessory muscles
Remember -
Absence of symptoms at the time of
examination does not exclude the
diagnosis of asthma
Dr.Sarma@works
21
Hyper-expansion of the thorax
Increased nasal secretions or
nasal polyps
Atopic dermatitis, eczema, or
other allergic skin conditions
PHYSICAL EXAM
Dr.Sarma@works
22
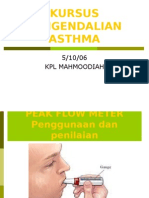
SCREENING TEST
Diagnosis of asthma can be suspected by
demonstrating the presence of airway
obstruction using Peak flow meter.
Peak Flow Meter is a basic
tool in a GPs office
PEFR amplitude ?
Dr.Sarma@works
23
DIAGNOSTIC TEST
Diagnosis of asthma can be
confirmed by demonstrating
the presence of reversible
airway obstruction using
Spirometry.
Dr.Sarma@works
24
SPIROMETRY
Let me now take you through to
the understanding of the basics
of spirometry
Dr.Sarma@works
25
SPIROMETRY
Basic Issues
Dr.Sarma@works
26
LUNG FUNCTION TESTS
Tests of Ventilation
Tests of Diffusion
Tests of Perfusion
Tests for V-P
Mismatch
Dr.Sarma@works
27
LUNG FUNCTION TESTS
Tests of Ventilation
Tests of Diffusion
Tests of Perfusion
Tests for V-P
Mismatch
Dr.Sarma@works
28
VENTILATION
Peak Expiratory Flow Rate
Simple, Peak flow meter is used
Flow volume loop , Flow time
curve
Detailed, Spirometry is used
Dr.Sarma@works
29
PEAK FLOW METER
Diagnosis of ASTHMA or COPD can be
confirmed by demonstrating the presence
of airway obstruction using Spirometry.
Dr.Sarma@works
30
PEFR - Pros and Cons
Advantages
With in 1 to 2 minutes,
Inexpensive (meter costs less than Rs.1000)
Simple, useful for frequent follow up use
Disadvantages
Very much effort dependent
Insensitive to small changes
Small airways cannot be assessed
Large inter & intra subject variation;accurate
Dr.Sarma@works
31
SPIROMETRY
Dr.Sarma@works
32
Spirometry - Pros and Cons
Advantages
Evaluates smaller as well as larger airways
Relatively easy to use and maintain
Reversibility can be tested with IBD and steroids
Diagnostic as well as management assessments
Disadvantages
Cost about 50,000 + computer and printer
Takes time to perform 10 to 15 minutes
Requires training at least one day course
Dr.Sarma@works
33
Spirometry Maneuver
In single breath test
A few normal tidal respirations
Then deeeeep inspiration
Momentary breath holding
Very forced and fast expiration
As hard and as fast as he/she can blow out
Then deep, quick and full inspiration
Repeat at least 3 times take the best
Dr.Sarma@works
34
Spirometry Results
FVC Forced Vital Capacity
FEV1 Forced Expiratory Volume
in the first second
FEV1FVC Ratio of the above two
PEFR Peak Expiratory Flow Rate
FET Forced Expiratory Time
Dr.Sarma@works
35
Spirometry Normal Values
1. There are no fixed Normal values
2. Dependent on age, sex, ht, wt, ethnicity
3. Observed value expressed as predicted value %
FVC Normal if > 80% of predicted
FEV1 Normal if > 80% of predicted
FEV1/FVC At least 75%
PEFR Normal if > 80% of predicted
FET Less than 4 seconds
Dr.Sarma@works
36
Obstructive v/s Restrictive
Parameter Normal Obstructive Restrictive
Problem Air out and
Air in normal
Unable to get
Air out
Unable to get
Air in
FVC 80 % of pred Normal or ,TLC
FEV1 80 % of pred -80% or less Normal
FEV1 FVC Min. of 75% -70% or less Normal or
PEFR 80 % of pred -80% or less Normal
FET in sec Less than 4 Prolonged > 4 Normal - < 4
Dr.Sarma@works
37
Flow-Volume, Volume-Time Graphs
Dr.Sarma@works
38
Normal Flow-Volume Loop
Dr.Sarma@works
39
Flow-Volume Loop in disease
Mild reversible obstruc Severe irreversible obstr Severe restrictive dis
ASTHMA COPD ILD
Dr.Sarma@works
40
Office Spirometry
Dr.Sarma@works
41
BACK TO ASTMA
Now, with this understanding of
spirometry, let us proceed to look
at the management of Asthma
Dr.Sarma@works
42
CLASSIFICATION OF SEVERITY
STEP 4
Severe
Persistent
STEP 3
Moderate
Persistent
STEP 2
Mild
Persistent
STEP 1
Intermittent
The presence of one of the features of severity is sufficient to place
a patient in that category.
Global Initiative for Asthma (GINA) WHO/NHLBI, 2002
Symptoms
Nighttime
Symptoms
FEV1
CLASSIFY SEVERITY
Clinical Features Before Treatment
Continuous
Limited physical
activity
Daily
Use b2-agonist
daily
Attacks affect
activity
>1 time a week
but <1 time a day
< 1 time a week
Asymptomatic
and normal PEF
between attacks
Frequent
>1 time week
>2 times a month
<2 times a month
<60% predicted
Variability >30%
>60%-<80%
predicted
Variability >30%
>80% predicted
Variability 20-
30%
>80% predicted
Variability <20%
Dr.Sarma@works
43
GOALS IN ASTHMA CONTROL
Achieve and maintain control of symptoms
Prevent asthma episodes or attacks
Minimal use of reliever medication
No emergency visits to doctors or hospitals
Maintain normal activity levels, including
exercise
Maintain pulmonary function as close to normal
as possible
Minimal (or no) side effects from medicine
Dr.Sarma@works
44
TOOL KIT WE HAVE
Relievers (Quick)
Preventers (long term)
Peak Flow meter
Spirometry
Patient education
Dr.Sarma@works
45
ASTHMA Rx. in INDIA TOADAY
Completely control symptoms and
Make their life normal
As good as abroad (even better)
General practice physicians
Doesnt need Chest Physicians !
Dr.Sarma@works
46
IT IS A DUAL PROBLEM
1. Bronchial inflammation perpetual
1. Allergic inflammation and edema
2. Inflammatory mediators perpetuate
3. edema and excite bronchospasm
4. Bronchial hyper reactivity to triggers
2. Bronchospasm acute attacks
This needs two different types of
medicines relievers & preventers
Dr.Sarma@works
47
WHAT ARE RELIEVERS ?
Spasm needs reliever
Bronchodilator drugs
Rescue medications
Quick relief of symptoms
Used during acute attacks
Action lasts for 4-6 hrs
Not for regular use at all
Dr.Sarma@works
48
RELIEVERS
Short acting b
2
agonists - SABA
Salbutamol, Terbutaline
Levo-salbutamol (Levolin)
Anti-cholinergics
Ipatropium
Xanthines
Theophylline (Deriphyllin group)
Dr.Sarma@works
49
Prevent future attacks
Reduce allergic inflammation
Reduce inflammatory mediators
Reduce hyper-responsiveness
Long term control of asthma
Prevent airway remodeling
For regular use well or ill
WHAT ARE PREVENTERS ?
Dr.Sarma@works
50
PREVENTERS
Xanthines
Theophylline SR
Mast cell stabilizers
Sodium cromoglycate
Nedocromil sodium
Ketotifen, Ceterizine
Combinations
Salmeterol/Fluticasone
Formoterol/Budesonide
Salbutamol/Beclomethasone
Corticosteroids
Prednisolone, Betamethasone
Beclomethasone, Budesonide
Fluticasone
Long acting b2 agonists-LABA
Bambuterol, Salmeterol
Formoterol, Bambuderol
Anti-leukotrienes
Montelukast, Zafirlukast, Pranlukast
Dr.Sarma@works
51
CERTAIN ABBREVIATIONS
ICS Inhaled corticosteroids
IBD Inhaled bronchodilators
SABA Short acting agonists
LABA Long acting agonists
LTA Leukotrine antagonists
OCS Oral corticosteroids
SR Sustained release
AchB Acetyl choline blockers
Dr.Sarma@works
52
NEW APPROACHES
Omalizumab injection
Monoclonal antibody against
Immunoglobin E (anti-IgE)
Monoclonal antibody to block
the allergic antibody, IgE
Dr.Sarma@works
53
PLEASE REMEMBER
If our patient uses reliever medication
every day, or even more than three or
four times a week, preventer medication
must be added to the treatment plan and
reliever medication has to be with drawn.
GINA Workshop Report,
December 2000
Dr.Sarma@works
54
Are we giving the right drug ?
Are we giving the drug in right form ?
Are we using the correct technique ?
LET US QUESTION
Dr.Sarma@works
55
WHAT HAPPENS WITH WRONG Rx. ?
Normal
Inflamed
(Asthma)
Partly Treated
Fixed Obstruction
(Lead Pipe)
Remodelled
Airway
Dr.Sarma@works
56
THE STORY OF ASTHMA TREATMENT
Normal
Regular
Inhaled
Steroid
Partly
Treated
Inflamed (untreated)
Remodeled
Dr.Sarma@works
57
All Asthma drugs should ideally be
taken through the inhaled route.
MOST IMPORTANT
Dr.Sarma@works
58
WHAT CHANGES THEIR LIFE ?
ICS are the most potent and effective
anti-inflammatory medication currently
available for Asthma *
*GINA (NHLBI & WHO Workshop Report), December 1995
*Guidelines for the diagnosis and management of Asthma NIH,
NHLBI, May 1997
ICS
Inhaled corticosteroids
Dr.Sarma@works
59
Corticosteroids ??
Inhaled medicines ??
LET US BELIEVE FIRST
Patients wrong belief
Parents / Grand parents
Neighbours / friends
First of all, let us believe in science
Let us explain and convince them
Let us change their lives to happy lives
Dr.Sarma@works
60
Instead of asthma controlling
our patient
REMEMBER
allow our patient to
control his / her asthma
Dr.Sarma@works
61
WHY INHALATION Rx.
Oral
Slow onset of action
Large dosage used
Greater side effects
Erratic absorption
Not useful in acute
illness
Inhaled route
Rapid onset of action
Less amount of drug
Drug delivered to
the site of mischief
Better tolerated
Treatment of choice
in acute symptoms
Dr.Sarma@works
62
PREVENTERS
Inhaled corticosteroids
Budesonide/ beclomethasone/
fluticasone use any
Start (400-1000 mcg/day approx. in
2 divided doses)
Maintain for 3 months
Taper slowly and keep at 200 mcg
Safe for long-term use (years)
Dr.Sarma@works
63
They are very safe
Even in small children for several years
30% of Olympic athletes use ICS
Not anabolic (performance-enhancing)
steroid
Even highest ICS dose is safer than low
dose oral steroid or beta agonist
Best Addiction for asthmatics
ICS HOW SAFE ?
Dr.Sarma@works
64
ICS SAFE EVEN FOR A CHILD?
400 mcg/day (budesonide)
Over 9 years of continuous use
No growth retardation
Uncontrolled asthma causes growth
retardation
Pedersen & Agertoft NEJM 2000
Dr.Sarma@works
65
PREGNANCY AND ASTHMA
Dont x-ray (if possible)
All asthma medication is safe
Even oral corticosteroids are safe for
exacerbations
Uncontrolled asthma during pregnancy
is a serious risk factor for foetal distress
and anoxia
Thorax Supplement
Dr.Sarma@works
66
ICS not Effective ?
Check Inhaler
Technique /
Check Regular
Use
Add LABA
Formoterol /
Salmeterol
Increase dose
of inhaled
steroid
Add Leukotriene
modifier
Add SR
Theophylline
Dr.Sarma@works
67
Step up and down - ACUTE
SABA (IBD) in full doses
SABA Increase frequency or Nebulize
SABA as above + IPA (IBD), then add
OCS (Prednisolone) 30-60 mg for 3 to 10 days - add
ICS (1000 mcg) / day and maintain for 6 weeks minimum
Gradually bring down doses and maintain with ICS
If symptoms are not relieved
Check the technique and the compliance with Rx.
Look for aggravating factors like
GE Reflux, Emotions/ stress, Sinusitis
Allergic Rhinitis, Persistent allergens
No role for Theophylline; Oral SABA or LABA not very useful
Dr.Sarma@works
68
The Step Care Approach - Prevent
ICS
ICS + LABA (IBD)
ICS + LABA (IBD) + Double Dose ICS
ICS (DD) + LABA + LTA (oral)
ICS (DD) + LABA + LTA + OCS
ICS (DD) + LABA + LTA + OCS + TIO (IBD)
SR Theophylline may be add on
SABA or LABA Oral + IPA (IBD) may be useful add on
No long acting steroid injections
No injectable or short acting Theophylline
Dr.Sarma@works
69
Leukotriene Modifiers
Oral leukotrine antagonist anti inflammatory
Not as effective as inhaled steroid
May be first-line for 2 to 5 yr. olds.
Montelukast available; Zafirlukast is not in India
4 mg, 5 mg, 8 mg tabs available
Can be add on to ICS, IBD inhalers
Dr.Sarma@works
70
NOT ALL ARE SAME !!
Beclomethasone 6 hrly + Salbutamol 6
th
hrly
Budesonide 12 hrly + Salmeterol 12 hrly
Salmeterol 12 hrly + Ipatropium 12 hrly
Fluticasone 24 hrly + Formoterol 24 hrly
Formoterol 24 hrly + Tiotropium 24 hrly
Choice is based on
1. If need is urgent and uncontrolled 6 hrly
2. If need is maintenance, well contr. 12 hrly
3. If stabilized and wants convenience 24 hrly
Dr.Sarma@works
71
Formoterol + Budesonide
combination - the Flexible Preventer
A
s
t
h
m
a
s
i
g
n
s
Time
2x2
2x2
1x1
1x2
1x2
Quickly
gains control
Maintains
control
Asthma
worsening
Maintains
control
Reduce to
lowest
adequate
dose that
maintains
control
Dr.Sarma@works
72
Why doctors dont use
inhalation therapy
Status quo :
my practice is good or great
Oral therapy is easy
Too busy
Difficulty in convincing
Cost
Headache to explain
Dr.Sarma@works
73
DRUG DELIVERY OPTIONS
Metered dose inhalers (MDI)
Dry powder inhalers (Rotahaler)
Spacers / Holding chambers
Nebulizers
Dr.Sarma@works
74
Demonstration of
the correct technique
Ask the patient to demonstrate to
you the technique
Dr.Sarma@works
75
pMDI Metered Dose Inhalers
Rotahalers, Diskhalers
Spacehalers
Nebulizers
Oxygen mixed delivery
Oral tablets, syrups
Parenteral I.M or I.V use
1. Dexterity
2. Hand grip strength
3. Co-ordination
4. Severity of COPD
5. Educational level
6. Age of the patient
7. Ability to inhale and
synchronize
DRUG DELIVERY - OPTIONS
Dr.Sarma@works
76
WHAT DRUG DELIVERY METHOD ?
Very young or very old MDI + LV Spacer
Elderly MDI + SV spacer
Young children > 7 yrs DPI (Rotahaler)
Adults edu. understood MDI alone
Adults no co-ordination DPI (Rotahalers)
Clinic setting MDI + Spacer
Clinic - emergency Nebulizer
Choice is to be individualized
Trial and error may be needed
Cost may be a factor
Dr.Sarma@works
77
DRUG DELIVERY - OPTIONS
Dr.Sarma@works
78
Spacer
Spacehaler
Rotahaler
Dry powder Inhaler
Metered dose
inhaler or MDI
INHALATION DEVICES
Dr.Sarma@works
79
MDI + LARGE VOLUME SPACER
Dr.Sarma@works
80
ROTAHALER DRY POWDER
Overcomes hand-lung coordination
problems encountered with MDIs.
Can be easily used by children, elderly and
arthritic patients.
Can take multiple inhalations if the entire
drug has not been inhaled in one inhalation.
Dr.Sarma@works
81
THE ZEROSTAT ADVANTAGE
1. Non - static spacer made up of polyamide material
2. Increased respirable fraction Increased deposition of
drug in the airways
3. Increased aerosol half - life Plenty of time for the
patient to inhale after actuation of the drug
4. No valve No dead space Less wastage of the drug
5. Small, portable, easy to carry Child friendly
Dr.Sarma@works
82
DISKHALER NEBULISER
Dr.Sarma@works
83
NEBULISED THERAPY
1. Severe breathlessness despite using inhalers
2. Assessment should be done for improvement
3. Choice between a facemask or mouth piece
4. Equipment servicing and support are essential
5. Dosage 0.5 ml of Ipatropium +
0.5 ml of Salbutamol + 5 ml of NaCl (not DW)
6. If decided to use ICS (FEV1 < 50%)
0.5 ml of Budusonide is added to the above
6. 15 minutes and slow or moderate flow rate
7. Can be repeated 2 to 3 times a day Mouth Wash
Dr.Sarma@works
84
PATIENT EDUCATION
Explain nature of the disease (inflammation)
Explain action of prescribed drugs
Stress the need for regular, long-term therapy
That way only we can convince
Allay fears and concerns
Peak flow testing
Symptom, treatment diary
Dr.Sarma@works
85
PATIENT EDUCATION
Asthma is a common disorder
It can happen to anybody, May not be life long
It is not caused by supernatural forces
Asthma is not contagious, All kin neednt be affected
Recurrent attacks of cough with or without wheeze
Between attacks people with asthma lead normal
lives as anyone else
In most cases, there is some family history of allergy
Dr.Sarma@works
86
Asthma can be effectively controlled, although it
cannot be cured.
Effective asthma management programs include
education, objective measures of lung function,
environmental control, and pharmacologic therapy.
A stepwise approach to pharmacologic therapy is
recommended. The aim is to accomplish the goals
of therapy with the least possible medication.
PATIENT EDUCATION
Dr.Sarma@works
87
A little time spent talking
to our patients - really
is a great investment.
This may make all the difference
between a happy life and
pulmonary invalidity
YOURS FAITHFULLY REQUESTS
Dr.Sarma@works
88
Can We dare to make
them pulmonary invalids ?
LET US GIVE THEM
LIFE TIME HAPPINESS
Você também pode gostar
- GP Reg - Asthma and Spirometry 2011Documento114 páginasGP Reg - Asthma and Spirometry 2011minerva_stanciuAinda não há avaliações
- Oxygenation Problem Notes and Nursing InterventionsDocumento7 páginasOxygenation Problem Notes and Nursing InterventionsAnna TaylorAinda não há avaliações
- PFT Tests Measure Lung FunctionDocumento19 páginasPFT Tests Measure Lung FunctionAshenafi BerhanuAinda não há avaliações
- 2.3 علاج تنفسى د كريم (1) -٣Documento11 páginas2.3 علاج تنفسى د كريم (1) -٣Ahmed KadiraAinda não há avaliações
- Spirometry Instructions HandoutDocumento3 páginasSpirometry Instructions HandoutJathurshika VigneswaranAinda não há avaliações
- GINA 2014 ShortcutDocumento44 páginasGINA 2014 ShortcutKath Dellosa100% (1)
- Emphysema Case Study AnalysisDocumento10 páginasEmphysema Case Study AnalysisEfren VisteAinda não há avaliações
- 1 CPG Asthma GuidelinesDocumento19 páginas1 CPG Asthma GuidelinesShofiyyatunnisa' WsAinda não há avaliações
- Pneumonia Case StudyDocumento24 páginasPneumonia Case StudyDharylle Cariño100% (1)
- Spirometry: Performance and Interpretation A Guide For General PractitionersDocumento15 páginasSpirometry: Performance and Interpretation A Guide For General PractitionersAgi AngloSaxonAinda não há avaliações
- Bronchial Asthma: CC Ayanne Aborka West Visayas State University Medical CenterDocumento71 páginasBronchial Asthma: CC Ayanne Aborka West Visayas State University Medical CenterAyanne AborkaAinda não há avaliações
- Define AsthmaDocumento5 páginasDefine Asthmatimie_reyesAinda não há avaliações
- BM Project On SpirometerDocumento11 páginasBM Project On SpirometerAnushka NardeAinda não há avaliações
- Respiratory Disorder Note BSC 3rd YearDocumento41 páginasRespiratory Disorder Note BSC 3rd YearNancyAinda não há avaliações
- Asthma : By: Mary Joseph Bitgue BSN 4ADocumento13 páginasAsthma : By: Mary Joseph Bitgue BSN 4AKaryn Joy LamisAinda não há avaliações
- Nicu Survival Guide For ResidentsDocumento26 páginasNicu Survival Guide For ResidentspeppepagAinda não há avaliações
- Spirometry Pulmonary Function TestDocumento17 páginasSpirometry Pulmonary Function TesthoohooAinda não há avaliações
- Seminar Asthma PDFDocumento39 páginasSeminar Asthma PDFAriff Mahdzub0% (1)
- Wear protective clothing to avoid secondary contaminationDocumento46 páginasWear protective clothing to avoid secondary contaminationyousernameAinda não há avaliações
- Asthma: Rochelle M. Nolte, MD CDR Usphs Family MedicineDocumento56 páginasAsthma: Rochelle M. Nolte, MD CDR Usphs Family MedicineJoan Marie Lechado InoviaAinda não há avaliações
- Seminar On AsthmaDocumento27 páginasSeminar On Asthmalumina.s100% (1)
- Monitor the patient closely and adjust settings as needed based on their responseDocumento61 páginasMonitor the patient closely and adjust settings as needed based on their responseVarun PatelAinda não há avaliações
- Deborah Hellyer AsthmaDocumento86 páginasDeborah Hellyer AsthmaGiorgi PopiashviliAinda não há avaliações
- Asthma For PTDocumento52 páginasAsthma For PTAnn SibyAinda não há avaliações
- Acute Lung Injury/Acute Respiratory Distress Syndrome: Deepak Mulajker, Vasu Vardhan, AK NagpalDocumento6 páginasAcute Lung Injury/Acute Respiratory Distress Syndrome: Deepak Mulajker, Vasu Vardhan, AK NagpalDeepak MulajkerAinda não há avaliações
- Respi Update 2019 SpirometryDocumento48 páginasRespi Update 2019 SpirometryJashveerBedi100% (1)
- Cough, Cold and AllergiesDocumento68 páginasCough, Cold and AllergiesLeonardo RanderAinda não há avaliações
- Pedia Bronchial Asthma-1Documento43 páginasPedia Bronchial Asthma-1MAHEJS HDAinda não há avaliações
- Influenza Common Colds OutputDocumento8 páginasInfluenza Common Colds OutputmalindaAinda não há avaliações
- Pocket Guide For Asthma Management and PreventionDocumento30 páginasPocket Guide For Asthma Management and PreventionAzu Sta MaríaAinda não há avaliações
- 01 05 05 Occs10080)Documento7 páginas01 05 05 Occs10080)IJIRAE- International Journal of Innovative Research in Advanced EngineeringAinda não há avaliações
- Pulmonary Function Test: By: Alfaro, Ruby Jane SDocumento13 páginasPulmonary Function Test: By: Alfaro, Ruby Jane SgjevamAinda não há avaliações
- Understanding Spirometry: Diagnosing and Monitoring Lung DiseaseDocumento68 páginasUnderstanding Spirometry: Diagnosing and Monitoring Lung Diseasex22xAinda não há avaliações
- RespiratoryDocumento17 páginasRespiratorykurutalaAinda não há avaliações
- AsthmaDocumento23 páginasAsthmaLeoAinda não há avaliações
- The PFT LexiconDocumento3 páginasThe PFT Lexiconjmel67Ainda não há avaliações
- Spirometris Con Enfoque ClínicoDocumento7 páginasSpirometris Con Enfoque ClínicomariaAinda não há avaliações
- Segui NCPDocumento4 páginasSegui NCPRichelle TalaguitAinda não há avaliações
- COVID-19, Severe Pneumonia, Diabetes, HCVDDocumento72 páginasCOVID-19, Severe Pneumonia, Diabetes, HCVDJUVIELY PREMACIOAinda não há avaliações
- Spiro Me Try Cheat Sheet 09Documento2 páginasSpiro Me Try Cheat Sheet 09Yudha Perwira PutraAinda não há avaliações
- Pulmonary Function Test, JARA CSUDocumento73 páginasPulmonary Function Test, JARA CSUJohn NicoleAinda não há avaliações
- 48 SpirometryDocumento18 páginas48 SpirometryZeeshan AhmadAinda não há avaliações
- Asthma and COPDDocumento79 páginasAsthma and COPDDawit g/kidanAinda não há avaliações
- Spirometry For Diagnosis of CopdDocumento4 páginasSpirometry For Diagnosis of CopdriasaliAinda não há avaliações
- Asthma and Atopic Eczema Asthma and Atopic Eczema Asthma and Atopic Eczema Asthma and Atopic EczemaDocumento14 páginasAsthma and Atopic Eczema Asthma and Atopic Eczema Asthma and Atopic Eczema Asthma and Atopic EczemaTom Mallinson100% (1)
- 4 Bronchial AsthmaDocumento9 páginas4 Bronchial Asthmashanfiza_92Ainda não há avaliações
- Evaluation Checklist Case 7 Bronchial AsthmaDocumento7 páginasEvaluation Checklist Case 7 Bronchial AsthmaChristian MendiolaAinda não há avaliações
- lr5 - ILHAASHINI (012021090323) - Lab 5 DoneDocumento7 páginaslr5 - ILHAASHINI (012021090323) - Lab 5 DoneIlhaashini krishnanAinda não há avaliações
- Pulmonary Function TestDocumento7 páginasPulmonary Function Testgurneet kourAinda não há avaliações
- Asthma - Peak Flow MeterDocumento22 páginasAsthma - Peak Flow Meterapi-3729824100% (2)
- Childhood Asthma: Symptoms, Causes, Risk Factors & ManagementDocumento9 páginasChildhood Asthma: Symptoms, Causes, Risk Factors & ManagementJaved IqbalAinda não há avaliações
- AsthmaDocumento9 páginasAsthmaNiña Jemia CortezAinda não há avaliações
- Managing A Mechanically Ventilated PatientDocumento51 páginasManaging A Mechanically Ventilated PatientPeony03Ainda não há avaliações
- IPSA I Final ExamDocumento218 páginasIPSA I Final ExamJohnny MillsAinda não há avaliações
- Spiro Me TryDocumento18 páginasSpiro Me TryAreesha ArifAinda não há avaliações
- Pulmonary Function TestsDocumento7 páginasPulmonary Function Testspragna novaAinda não há avaliações
- ARDSDocumento57 páginasARDSnesjohnvAinda não há avaliações
- Pulmonary Function TestsDocumento24 páginasPulmonary Function TestsSachin KonkaniAinda não há avaliações
- Infectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersNo EverandInfectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersAinda não há avaliações
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseAinda não há avaliações
- Consumer Behavior: Importance in Pharmaceutical IndustryDocumento28 páginasConsumer Behavior: Importance in Pharmaceutical IndustrySurbhi JoshiAinda não há avaliações
- Social and Cultural EnvironmentDocumento30 páginasSocial and Cultural EnvironmentSurbhi JoshiAinda não há avaliações
- New Product Development MKTG 4320.002: Dr. Audhesh PaswanDocumento17 páginasNew Product Development MKTG 4320.002: Dr. Audhesh PaswanSurbhi JoshiAinda não há avaliações
- COMMDocumento29 páginasCOMMSurbhi JoshiAinda não há avaliações
- Effective Communication in The WorkplaceDocumento54 páginasEffective Communication in The WorkplaceBasile FistonAinda não há avaliações
- International Business Environment NotesDocumento0 páginaInternational Business Environment NotesSurbhi JoshiAinda não há avaliações
- Conflict ManagementDocumento22 páginasConflict ManagementcarloscanaisAinda não há avaliações
- Mr. Sudarshan Mrs. Phani Sirisha Ms. Payal Garg Mr. Yogesh Supekar Mr. Razz KumarDocumento14 páginasMr. Sudarshan Mrs. Phani Sirisha Ms. Payal Garg Mr. Yogesh Supekar Mr. Razz KumarSurbhi JoshiAinda não há avaliações
- Gpat 2014 SolvedDocumento12 páginasGpat 2014 Solvedjhansi100% (1)
- Trilead bis(carbonate) dihydroxide identified as SVHC due to reproductive toxicityDocumento7 páginasTrilead bis(carbonate) dihydroxide identified as SVHC due to reproductive toxicityCekinAinda não há avaliações
- John Taylor Case Study ENP and EPPDocumento11 páginasJohn Taylor Case Study ENP and EPPAhata Sham NewazAinda não há avaliações
- Ten Laws of BoundariesDocumento17 páginasTen Laws of Boundariesstjohn30067% (3)
- Tan Trok Tam Devi Suk TamDocumento4 páginasTan Trok Tam Devi Suk Tamtejasg82Ainda não há avaliações
- Stomach CancerDocumento19 páginasStomach CancerChristofer MadrigalAinda não há avaliações
- TVL ICT IllustrationNCII Q1Module2Documento12 páginasTVL ICT IllustrationNCII Q1Module2Kimberly Trocio Kim100% (1)
- Full Test 14 (Key) PDFDocumento4 páginasFull Test 14 (Key) PDFhoang lichAinda não há avaliações
- Evonik Copi BrochureDocumento5 páginasEvonik Copi BrochureRovshan HasanzadeAinda não há avaliações
- STRATEGIC MANAGEMENT FRAMEWORKDocumento19 páginasSTRATEGIC MANAGEMENT FRAMEWORKCharles CagaananAinda não há avaliações
- Low Back Pain Anatomy of Thoracolumbar SpineDocumento10 páginasLow Back Pain Anatomy of Thoracolumbar SpineMAinda não há avaliações
- Masagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningDocumento6 páginasMasagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningjhonaAinda não há avaliações
- ThesisDocumento26 páginasThesiscmomcqueenAinda não há avaliações
- Final Draft - Banana ChipsDocumento34 páginasFinal Draft - Banana ChipsAubrey Delgado74% (35)
- SITHCCC018 Assessment 2Documento9 páginasSITHCCC018 Assessment 2Taimoor Ahmed0% (1)
- Reduced Renal Sodium Excretion: Forced Through A Narrow LumenDocumento5 páginasReduced Renal Sodium Excretion: Forced Through A Narrow LumenFlowerAinda não há avaliações
- The Dukan Diet by Dr. Pierre Dukan - ExcerptDocumento8 páginasThe Dukan Diet by Dr. Pierre Dukan - ExcerptCrown Publishing Group15% (20)
- MSDS Summary: Naphtha VM&PDocumento6 páginasMSDS Summary: Naphtha VM&PRizki Adwitiyo 'Dito'Ainda não há avaliações
- Design and PlanningDocumento15 páginasDesign and PlanningZeljkoSipcicAinda não há avaliações
- Environmental Clearance CertificateDocumento4 páginasEnvironmental Clearance CertificateAra Jane T. PiniliAinda não há avaliações
- Design and Analysis of Cooling Fins: Deepak Gupta, Wankhade S.RDocumento4 páginasDesign and Analysis of Cooling Fins: Deepak Gupta, Wankhade S.RAntonio SilvaAinda não há avaliações
- How Time Management Impacts Working Students' Academic AchievementDocumento13 páginasHow Time Management Impacts Working Students' Academic AchievementJames RayAinda não há avaliações
- 2.9&10 Synthesis Adn Stereoisomerism Exam Qs - 4Documento4 páginas2.9&10 Synthesis Adn Stereoisomerism Exam Qs - 4sureshthevanAinda não há avaliações
- Test Bank For Leadership and Management in Nursing 4th Edition Mary Ellen Grohar MurrayDocumento36 páginasTest Bank For Leadership and Management in Nursing 4th Edition Mary Ellen Grohar Murraywitchingmazybs7k7100% (39)
- TLE Pre-Assessment Most & Least Learned SkillsDocumento7 páginasTLE Pre-Assessment Most & Least Learned SkillsRd DavidAinda não há avaliações
- Manufacturing ProcessDocumento6 páginasManufacturing Processbro nawalibmatAinda não há avaliações
- Electro BladeDocumento2 páginasElectro Bladeapi-19808945Ainda não há avaliações
- اللائحة التنظيمية لسفن الكروز - النسخة العربية - TransDocumento10 páginasاللائحة التنظيمية لسفن الكروز - النسخة العربية - TranssalsabilAinda não há avaliações
- Blessed Are Those Who MournDocumento7 páginasBlessed Are Those Who MournPatrick MabbaguAinda não há avaliações
- O-Rings & SealsDocumento10 páginasO-Rings & SealsPartsGopher.comAinda não há avaliações