Escolar Documentos
Profissional Documentos
Cultura Documentos
Anatomy of The Tongue
Enviado por
DrMohmd Zidaan0 notas0% acharam este documento útil (0 voto)
55 visualizações36 páginasThe tongue is a muscular organ located in the oral cavity. It has several parts including a dorsum, tip, inferior surface, and root. It is covered by mucous membrane and contains different types of papillae. Intrinsic and extrinsic muscles allow for movement and functions of the tongue like speech, swallowing and tasting. The tongue has blood, lymph and nerve supply to support its roles in the oral cavity.
Descrição original:
describes Tongue anatomy aided by photos
A mass of skeletal muscle covered by mucous membrane
Midline septum separating two muscular halves
Has dorsum, tip, inferior surface and root
Anterior 2/3 (oral part) - faces upwards towards the hard palate
Posterior 1/3 (pharyngeal part) - faces backwards towards the oropharynx
Stratified squamous epithelium:
keratinised on the oral part
non-keratinised on the pharyngeal part
Título original
Anatomy of the Tongue
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoThe tongue is a muscular organ located in the oral cavity. It has several parts including a dorsum, tip, inferior surface, and root. It is covered by mucous membrane and contains different types of papillae. Intrinsic and extrinsic muscles allow for movement and functions of the tongue like speech, swallowing and tasting. The tongue has blood, lymph and nerve supply to support its roles in the oral cavity.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
55 visualizações36 páginasAnatomy of The Tongue
Enviado por
DrMohmd ZidaanThe tongue is a muscular organ located in the oral cavity. It has several parts including a dorsum, tip, inferior surface, and root. It is covered by mucous membrane and contains different types of papillae. Intrinsic and extrinsic muscles allow for movement and functions of the tongue like speech, swallowing and tasting. The tongue has blood, lymph and nerve supply to support its roles in the oral cavity.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 36
Fuad Ridha Mahabot
A mass of skeletal muscle covered by mucous membrane
Midline septum separating two muscular halves
Has dorsum, tip, inferior surface and root
Anterior 2/3 (oral part) - faces upwards towards the hard
palate
Posterior 1/3 (pharyngeal part) - faces backwards towards the
oropharynx
Stratified squamous epithelium:
keratinised on the oral part
non-keratinised on the pharyngeal part
Tip - is the most anterior - merges into the inferior surface
Mucous membrane of the inferior surface - thin and smooth
(similar to FOM and cheek)
Oral anterior 2/3 of the dorsum of the tongue:
covered by mucous membrane into which underlying muscles are inserted
surface is roughened by the presence of 3 types of papillae: filiform,
fungiform and vallate papillae
Filiform papillae:
conical projections that give rise to velvety appearance of the
tongue
located along the entire dorsum of the tongue, but they are not
involved in taste sensation
Foliate papillae:
small folds of mucosa located along the lateral surface of the
tongue
Fungiform papillae:
visible as discrete pink pinheads
more numerous towards the edge of the tongue
each bears a few taste buds
Vallate papillae:
are about a dozen in number
arranged in the form of a V with apex pointing backwards
each is a cylindrical projection surrounded a circular sulcus and a
raised outer wall
there are many taste buds and serous glands in the sulcus that
surrounds each vallate papillae (as there are no other glands on
the dorsum of anterior 2/3 of the tongue)
Vallate Papillae
Fungiform Papillae
Filiform Papillae
sulcus terminalis: ill defined shallow groove which marks the
junction of the oral and the pharyngeal part of the tongue
vallate papillae are far back on the oral surface - not in contact
with the food being chewed; but the food juices and saliva reach
them - so flavours are transmitted to them
There are scattered mucous and serous glands under the tip and sides
On the undersurface behind the tip there is a rather large mixed gland on
the each side of midline - anterior lingual gland
From each gland small ducts open on the undersurface of the tongue
Ranula - retention cyst of this gland
Posterior 1/3 of the dorsum of the tongue:
is the anterior wall of the oropharynx
extends from sulcus terminalis and epiglottis
Foramen caecum: is a small depression at the apex of the sulcus - the
remains of the upper end of the thyroglossal duct
there are no papillae behind this sulcus
Smooth mucous membrane has a nodular appearance - constitute the
lingual tonsil, part of Waldeyers ring.
Between tongue and epiglottis - midline flange of mucous membrane
(median glossoepiglottic fold).
Each side of which is depression (valleculae), bounded laterally by
similar mucosal fold (lateral glossoepiglottic fold), extending from the
side of the epiglottis to the wall of the pharynx
Inferior surface of the tongue:
Lingual frenulum - a small midline septum of mucous membrane - unites it
to the floor of the mouth
Lateral to this - deep lingual vein (visible through the mucosa); lingual
artery and nerve (not visible)
Farther laterally is another fold of mucosa - fimbriated fold
Foliate papillae - a series of parallel folds of mucous membrane on the
sides of the posterior part of the tongue
Palatoglossal arches (anterior pillars of the pauces) - ridge of
mucous membrane raised up by palatoglossus muscles
extends from the undersurface of the front of the soft palate to the
sides of tongue in line with the vallate papillae
the whole constitutes oropharyngeal isthmus
closed by depression of the palate and elevation of dorsum of
tongue
narrowed by contraction of palatoglossus muscle
Divided into:
intrinsic (wholly within the tongue and not attached to the bone)
superior longitudinal
inferior longitudinal
transverse
vertical
extrinsic (attached to the bone)
genioglossus
hyoglossus
styloglossus
palatoglossus
Intrinsic Muscles
Superior longitudinal muscle:
lies beneath mucous membrane
shortens the tongue, make its dorsum concave
Inferior longitudinal muscle:
lying close to the inferior surface of the tongue
between genioglossus and hyoglossus
shortens the tongue, make its dorsum convex
Transverse muscle:
extends from median septum to the margins
makes the tongue narrow and elongated
Vertical muscle:
found at the borders of the anterior part of the tongue
makes the tongue broad and flattened
Extrinsic Muscles
Genioglossus:
origin: Upper genial tubercle of mandible
insertion: the fibres radiate widely to be inserted into the mucous
membrane of the tongue; the lowest fibres passing down to the hyoid
body
Hyoglossus:
origin: from the length of the greater horn of the hyoid bone and from
lateral part of its body
insertion: the fibres extend upward and its upper border
interdigitating at right angles with the fibres of styloglossus, and is
attached to the side of the tongue
Superficial to muscle from the above downwards:
lingual nerve
submandibular duct
hypoglossal nerve with its accompanying veins
Passing deep to its posterior border from above downwards:
glossopharyngeal nerve
styloid ligament
lingual artery
Styloglossus:
origin: from the front of the lower part of the styloid process and the
upper part of the stylohyoid ligament
insertion: passes forwards below the superior constrictor to be
inserted into the side of the tongue, interdigitating with upper fibres
of hyoglossus
Palatoglossus:
origin: arises from the undersurface of the palatine aponeurosis
insertion: side of the tongue (junction of oral and pharygeal part)
Muscles Origin Inserton Action(s)
Genioglossus
Upper genial tubercle
of mandible
Upper fibres: tip of
the tongue
Middle fibres: dorsum
Lower fibres: hyoid
bone
Upper fibres: retract the
tip
Middle fibres: depress the
tongue
Lower fibres: pull the
posterior part forward
(thus protrusion of the
tongue from the mouth)
Hyoglossus
Greater cornu, front
of lateral part of body
of hyoid bone
Side of tongue
Depress the tongue
Retracting the protruded
tongue
Styloglossus
Tip, anterior surface
of styloid process
Side of tongue
Pulls the tongue upwards
and backwards during
swallowing
Palatoglossus
Oral surface of
palatine aponeurosis
Side of tongue
(junction of oral and
pharygeal part)
Pulls up root of tongue,
approximates
palatoglossal arches,
closes oropharyngeal
isthmus
Tongue is supplied by the lingual artery
run above the greater horn of the hyoid bone deep to hyoglossus
passes forwards to the tip
beneath hyoglossus it gives off dorsal lingual branches into the
posterior part
at the anterior border of hyoglossus it gives a branch to the sublingual
gland and the floor of the mouth
fibrous septum dividing the two halves of the tongue prevents any
significant anastomosis of blood vessels across the midline
Venous tributaries
accompanying the lingual artery
its dorsal branches form the lingual vein
from the tip by deep lingual vein
it runs back superficial to hyoglossus and is joined at the anterior
border of the muscle by the sublingual vein (from the sublingual
gland) to form the vena comitans of the hyprglossal nerve
it continues backwards close to the nerve and joining either the
lingual, facial or internal jugular vein
lingual vein usually joins the internal jugular near the greater horn of
the hyoid bone
Lymph from one side (esp. of the posterior side), may reach
the nodes of the both sides of the neck (in contrast to the
blood supply which remains unilateral)
Tip - drain to submental nodes or directly to deep cervical
nodes
Marginal lymphatics from the anterior part tend to drain to
ipsilateral submandibular nodes or directly to deep cervical
nodes
Central lymphatics - drain to deep cervical nodes of either
side
Posterior part - drains directly and bilaterally to deep cervical
nodes
The deep cervical nodes usually involved: jugulodigastric and
jugulo-omohyoid nodes
All lymph from the tongue is believed to eventually drain
through the jugulo-omohyoid node before reaching the
thoracic duct or right lymphatic duct
Motor: all muscles of the tongue (intrinsic and extrinsic) are
supplied by hypoglossal nerve except palatoglossus which is
supplied by pharyngeal plexus
Sensory:
anterior 2/3 of the tongue:
general sensation: lingual nerve - branch of the mandibular nerve
(with cell bodies in the trigeminal ganglion)
taste: chorda tympani (with cell bodies in the geniculate ganglion
of facial nerve)
parasympathetic secretomotor fibres to the anterior lingual gland
run in the chorda tympani from the superior salivary nucleus, and
relay in the submandibular genglion
posterior 1/3 of the tongue: innervated by the glossopharyngeal
nerve (both general sensation and taste), with cell bodies in the
glossopharyngeal ganglia in the jugular foramen
posterior most part of the tongue: innervated by the vagus nerve
through the internal laryngeal branch (with cell bodies in the inferior
vagal ganglion)
Starts to develop near the end of the fourth week
Epithelium:
Anterior 2/3:
from 2 lingual swellings and one tuberculum impar, i.e., from first
branchial arch
supplied by lingual nerve (post-trematic) and chorda tympani (pre-
trematic)
Posterior 1/3:
from the cranial half of the hypobranchial eminence, i.e., from the
third arch
supplied by glossopharyngeal nerve
Posterior most:
from the fourth arch
supplied by vagus nerve
Muscles develop from the occipital myotomes which are
supplied by hypoglossal nerve
Connective tissue develops from local mesenchyme
Injury to hypoglossal nerve produces paralysis of the muscles
of the tongue on the side of lesion
infranuclear lesion (i.e., in motor neuron disease and in syringobulbia):
gradual atrophy and muscular twitchings of the affected half of the
tongue observed
supranuclear lesion (i.e., in pesudobulbar palsy): produce paralysis
without palsy (tongue is stiff, small and moves sluggishly)
The presence of rich networkof lymphatics and loose areolar
tissue in the substance of tongue is responsible for enormous
swelling of tongue in acute glossitis
The undersurface of the tongue is a good site for observation
of jaundice
In unconscious patients, the tongue may fall back and
obstruct the air passages. This can be prevented by lying the
patient on one side with head down or by keeping the tongue
pulled out mechanically
In the carcinoma of tongue, the affected site of tongue is
removed surgically. All deep cervical nodes are also removed
(block dissection)
Carcinoma of posterior 1/3 of the tongue is more dangerous
due to bilateral lymphatic spread
Você também pode gostar
- Physical Assessment Head To ToeDocumento4 páginasPhysical Assessment Head To ToeFely Theresa Lanes Loreno95% (43)
- HEENT ExamDocumento7 páginasHEENT Examnz0ptkAinda não há avaliações
- OutLines of European Board Exam-HNS - ExamDocumento19 páginasOutLines of European Board Exam-HNS - ExamDrMohmd ZidaanAinda não há avaliações
- Oral Cavity Is The Mirror of Your Own BodyDocumento60 páginasOral Cavity Is The Mirror of Your Own BodyNazia AliAinda não há avaliações
- Dent 355-10 Keratoses and Related Disorders of Oral MucosaDocumento23 páginasDent 355-10 Keratoses and Related Disorders of Oral MucosaHamna FitriahAinda não há avaliações
- Hairy TongueDocumento2 páginasHairy Tonguegodswar3dAinda não há avaliações
- The Normal Periodontium 1-GingivaDocumento34 páginasThe Normal Periodontium 1-GingivaHeba S Radaideh100% (1)
- Conversation Club Advanced Fortune Telling Predicting The FutureDocumento3 páginasConversation Club Advanced Fortune Telling Predicting The FutureWendy LittlefairAinda não há avaliações
- Periodontal AbscessDocumento40 páginasPeriodontal AbscessDrDebasish Mishra100% (1)
- Black Hairy Tongue: Simple Steps to Eliminate the ConditionNo EverandBlack Hairy Tongue: Simple Steps to Eliminate the ConditionAinda não há avaliações
- Periodontal MedicineDocumento24 páginasPeriodontal MedicineMoola Bharath Reddy100% (1)
- BASICS of ORAL PHYSIOLOGY (Part 1)Documento171 páginasBASICS of ORAL PHYSIOLOGY (Part 1)Balarabe EL-HussainAinda não há avaliações
- The Newest and Timeless Key for Anti-Aging Perfect for all Middle Aged PersonsNo EverandThe Newest and Timeless Key for Anti-Aging Perfect for all Middle Aged PersonsAinda não há avaliações
- Oral Leukoplakia: A ReviewDocumento60 páginasOral Leukoplakia: A ReviewdimasahadiantoAinda não há avaliações
- 100 Short Quotes from St. John Baptist De La SalleDocumento16 páginas100 Short Quotes from St. John Baptist De La SalleJayalakshmi V RamaduraiAinda não há avaliações
- Causes of Hearing Loss, Deafness, and Tinnitus/Ringing Ears - Information From NOWiHEAR ProfessionalsDocumento6 páginasCauses of Hearing Loss, Deafness, and Tinnitus/Ringing Ears - Information From NOWiHEAR Professionalscheerfulnecessi98Ainda não há avaliações
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Anatomy and Physiology MouthDocumento4 páginasAnatomy and Physiology MouthAndrew BimbusAinda não há avaliações
- Kant's Categorical Imperative: Morality as DutyDocumento57 páginasKant's Categorical Imperative: Morality as DutyAlyssa Marie SantosAinda não há avaliações
- Oral Hygiene Is NecessaryDocumento4 páginasOral Hygiene Is NecessaryRimsha KhanAinda não há avaliações
- Fuad Ridha MahabotDocumento36 páginasFuad Ridha MahabotLore DanAinda não há avaliações
- 14-Oral CavityDocumento37 páginas14-Oral CavitySajid AliAinda não há avaliações
- Oral Cavity585689409Documento37 páginasOral Cavity585689409mittal.shubham0007Ainda não há avaliações
- 14 Oral CavityDocumento41 páginas14 Oral Cavityhamokimo65Ainda não há avaliações
- TONGUEDocumento63 páginasTONGUEAthulya LakshmananAinda não há avaliações
- W2-8 Oral Region Lecture PDFDocumento69 páginasW2-8 Oral Region Lecture PDFSAHIL AGARWALAinda não há avaliações
- Anatomy of Oral CavityDocumento44 páginasAnatomy of Oral CavityRamesh ReddyAinda não há avaliações
- Oral CavityDocumento59 páginasOral CavityshaisidroAinda não há avaliações
- Tongue and PalateDocumento103 páginasTongue and PalateHeba S RadaidehAinda não há avaliações
- Amirhossein Vaezi MS121 Oral CavityDocumento27 páginasAmirhossein Vaezi MS121 Oral Cavityamirhossein vaeziAinda não há avaliações
- 14-ORAL CAVITY and Pharynx FinalDocumento50 páginas14-ORAL CAVITY and Pharynx FinalSudeep DhakalAinda não há avaliações
- Tongue Anatomy EssentialsDocumento15 páginasTongue Anatomy EssentialsArnab KalitaAinda não há avaliações
- Salivary Glands, The Oral Fissure and LipsDocumento53 páginasSalivary Glands, The Oral Fissure and LipsGeoffreyAinda não há avaliações
- Tongue IDocumento25 páginasTongue Igajendra ChoudharyAinda não há avaliações
- TONGUE Seminar by MeDocumento84 páginasTONGUE Seminar by MeArpita SankhwarAinda não há avaliações
- Tongue IDocumento25 páginasTongue IJohn SmithAinda não há avaliações
- ANATOMY ORAL CAVITY and TONGUE JelDocumento54 páginasANATOMY ORAL CAVITY and TONGUE JelCoy EnAinda não há avaliações
- TONGUE SeminarDocumento82 páginasTONGUE SeminarArun MamachanAinda não há avaliações
- Anatomi Dan Fisiologi Mulut Bp2Documento47 páginasAnatomi Dan Fisiologi Mulut Bp2Aditya FirmansyahAinda não há avaliações
- Oral CavityDocumento20 páginasOral CavityadileidalaaAinda não há avaliações
- Anatomy of Tongue and Its Applied Aspects: Presented By: Niti SarawgiDocumento77 páginasAnatomy of Tongue and Its Applied Aspects: Presented By: Niti SarawgideepAinda não há avaliações
- Mulut, Faring, LaringDocumento76 páginasMulut, Faring, LaringNiddy Rohim FebriadiAinda não há avaliações
- Anatomy Histology of The Oral Cavity2 3Documento31 páginasAnatomy Histology of The Oral Cavity2 3drsondosAinda não há avaliações
- Anatomi Trias Mengisap, Menelan dan BernapasDocumento74 páginasAnatomi Trias Mengisap, Menelan dan BernapasAnonymous KrEomRrAinda não há avaliações
- Anatomy of AirwaysDocumento6 páginasAnatomy of Airwaysgdubs215Ainda não há avaliações
- TongueDocumento46 páginasTonguedeepak mauryaAinda não há avaliações
- Role of Tongue N Floor of Mouth in CD TRTDocumento18 páginasRole of Tongue N Floor of Mouth in CD TRTashoorocksAinda não há avaliações
- Oral CavityDocumento98 páginasOral CavitynicewanAinda não há avaliações
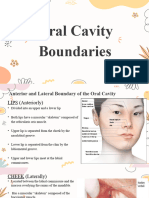
- Oral Cavity BoundariesDocumento8 páginasOral Cavity BoundariesLean Edrielle BillonesAinda não há avaliações
- TongueDocumento44 páginasTongueSidhartha BordoloiAinda não há avaliações
- TongueDocumento52 páginasTongueNANDANA BOSEAinda não há avaliações
- Accessory Organs of The Git - Gross AnatomyDocumento172 páginasAccessory Organs of The Git - Gross AnatomyManisha RaoAinda não há avaliações
- TongueDocumento10 páginasTongueBhuwanesh SharmaAinda não há avaliações
- 4TONGUEDocumento15 páginas4TONGUEZakaria Abdul HafizAinda não há avaliações
- Tongue and Its Role in Pros Tho Don TicsDocumento100 páginasTongue and Its Role in Pros Tho Don TicsDr Mohit Dhawan100% (18)
- Lecture 64: Anatomy of Tongue: Dr. Mohammad Rehan AsadDocumento20 páginasLecture 64: Anatomy of Tongue: Dr. Mohammad Rehan AsadRehan Asad0% (1)
- Oral Cavity AnatomyDocumento40 páginasOral Cavity AnatomyharisAinda não há avaliações
- Tongue and Its MusculatureDocumento89 páginasTongue and Its MusculaturedrsanketcAinda não há avaliações
- The TongueDocumento7 páginasThe Tonguemanojchouhan2014Ainda não há avaliações
- Tongue & It's Applied AspectsDocumento64 páginasTongue & It's Applied AspectsPrachi MulayAinda não há avaliações
- 14-Oral CavityDocumento30 páginas14-Oral CavityNeeta ChhabraAinda não há avaliações
- Neck Dissection PPs PresentationDocumento139 páginasNeck Dissection PPs PresentationDrMohmd ZidaanAinda não há avaliações
- Key Topics ENTDocumento375 páginasKey Topics ENTanas_marzoukAinda não há avaliações
- Auto Mastoid EctomyDocumento1 páginaAuto Mastoid EctomyDrMohmd ZidaanAinda não há avaliações
- Young Child With Cystic Fibrosis and SinonasalDocumento5 páginasYoung Child With Cystic Fibrosis and SinonasalDrMohmd ZidaanAinda não há avaliações
- Facial FlapsDocumento72 páginasFacial FlapsDrMohmd Zidaan100% (1)
- Grading Systems in Head and Neck DysplasiaDocumento8 páginasGrading Systems in Head and Neck DysplasiaDrMohmd ZidaanAinda não há avaliações
- Facial FlapsDocumento72 páginasFacial FlapsDrMohmd Zidaan100% (1)
- Development of Minimally Invasive Surgery SystemsDocumento7 páginasDevelopment of Minimally Invasive Surgery SystemsDrMohmd ZidaanAinda não há avaliações
- Oro Antral CommunicationDocumento6 páginasOro Antral CommunicationPorcupine TreeAinda não há avaliações
- Causing SymptomsDocumento2 páginasCausing SymptomskurutalaAinda não há avaliações
- Primary Care Otolaryngology OnlineDocumento212 páginasPrimary Care Otolaryngology OnlineDrMohmd ZidaanAinda não há avaliações
- Systematic Facial Nerve Monitoring in Middle Ear and Mastoid Surgeries - Surgical Dehiscence - and - Electrical DehiscenceDocumento5 páginasSystematic Facial Nerve Monitoring in Middle Ear and Mastoid Surgeries - Surgical Dehiscence - and - Electrical DehiscenceDrMohmd ZidaanAinda não há avaliações
- Assessment of Eustachian Tube Function in TympanoplastyDocumento5 páginasAssessment of Eustachian Tube Function in TympanoplastyDrMohmd ZidaanAinda não há avaliações
- Perception-Based Protection From Low-Frequency Sounds May Not Be EnoughDocumento12 páginasPerception-Based Protection From Low-Frequency Sounds May Not Be EnoughDrMohmd ZidaanAinda não há avaliações
- Tympanoplasty Excellent Summary1Documento29 páginasTympanoplasty Excellent Summary1DrMohmd ZidaanAinda não há avaliações
- Perception-Based Protection From Low-Frequency Sounds May Not Be EnoughDocumento12 páginasPerception-Based Protection From Low-Frequency Sounds May Not Be EnoughDrMohmd ZidaanAinda não há avaliações
- Technical Instructions For TuberculosisDocumento33 páginasTechnical Instructions For TuberculosisDrMohmd ZidaanAinda não há avaliações
- Pediatric OtolaryngologyDocumento242 páginasPediatric OtolaryngologyDrMohmd ZidaanAinda não há avaliações
- ENT Syndromes Glasgow 2009Documento41 páginasENT Syndromes Glasgow 2009DrMohmd ZidaanAinda não há avaliações
- Assessment of Eustachian Tube Function in TympanoplastyDocumento5 páginasAssessment of Eustachian Tube Function in TympanoplastyDrMohmd ZidaanAinda não há avaliações
- Dr. Zidan ProofDocumento11 páginasDr. Zidan ProofDrMohmd ZidaanAinda não há avaliações
- MY VocabularyDocumento25 páginasMY VocabularyDrMohmd ZidaanAinda não há avaliações
- Endoscopic Closure of CSF Rhinorrhea-193 Cases Over 21 YearsDocumento8 páginasEndoscopic Closure of CSF Rhinorrhea-193 Cases Over 21 YearsDrMohmd ZidaanAinda não há avaliações
- Epistaxis 111127170402 Phpapp01Documento27 páginasEpistaxis 111127170402 Phpapp01DrMohmd ZidaanAinda não há avaliações
- DPT SyllabusDocumento277 páginasDPT Syllabusshahidmahboob60100% (1)
- Surgical Pathology - English CourseDocumento675 páginasSurgical Pathology - English Coursedidutza91100% (1)
- CARDIO ANAT and EMBRYO Da SouzaDocumento18 páginasCARDIO ANAT and EMBRYO Da Souzagaza slimAinda não há avaliações
- Head and Neck TumorsDocumento14 páginasHead and Neck TumorsBarda GulanAinda não há avaliações
- Kundalini Yogafor The Liver, Colon and StomachDocumento4 páginasKundalini Yogafor The Liver, Colon and StomachSandra Costa Bras100% (1)
- Deep Neck AbscessDocumento39 páginasDeep Neck AbscessCarmelli Mariae CalugayAinda não há avaliações
- Penetrating Neck Injuries GuideDocumento8 páginasPenetrating Neck Injuries GuideAyesh EKAinda não há avaliações
- Physical assessment findings 55kg womanDocumento5 páginasPhysical assessment findings 55kg womanMtch V. BumanlagAinda não há avaliações
- OJSimpson Case StudyDocumento30 páginasOJSimpson Case StudyhksmartAinda não há avaliações
- Important Topics Checklist For NEET PG - Anatomy: From DR Ankit KhandelwalDocumento11 páginasImportant Topics Checklist For NEET PG - Anatomy: From DR Ankit KhandelwalYuku BabyAinda não há avaliações
- Name of Exercise Area (S) of Body Imbalance (S) Structures AddressedDocumento2 páginasName of Exercise Area (S) of Body Imbalance (S) Structures AddressedBruce HoAinda não há avaliações
- Head, Eyes, Ears, Nose, Mouth and Throat ExamDocumento2 páginasHead, Eyes, Ears, Nose, Mouth and Throat ExamMae DoctoleroAinda não há avaliações
- To Begin: MantraDocumento9 páginasTo Begin: MantraashissahooAinda não há avaliações
- PATIENT POSITIONING AND ANAESTHESIA SAFETYDocumento24 páginasPATIENT POSITIONING AND ANAESTHESIA SAFETYGrishma KothariAinda não há avaliações
- Levels of cervical lymph nodesDocumento4 páginasLevels of cervical lymph nodesSaleh SaqerAinda não há avaliações
- Romanian JournalDocumento60 páginasRomanian JournalLocalitatea BabadagAinda não há avaliações
- Asana Postures - Swami VishnudevanandaDocumento83 páginasAsana Postures - Swami VishnudevanandatrankimbaonkvAinda não há avaliações
- IELTS Reading Test 1Documento13 páginasIELTS Reading Test 1SurikaAinda não há avaliações
- Neck Dissection: Presenter Dr. Dessalegn.B. (ENT RIII) Moderater DR - Nitin (OMF Surgeon)Documento67 páginasNeck Dissection: Presenter Dr. Dessalegn.B. (ENT RIII) Moderater DR - Nitin (OMF Surgeon)johnAinda não há avaliações
- Centro Escolar University Nursing Department Malolos City, BulacanDocumento5 páginasCentro Escolar University Nursing Department Malolos City, BulacanBee Anne BiñasAinda não há avaliações
- Chakras Book FromDocumento22 páginasChakras Book FromLindsey SpencerAinda não há avaliações
- Head Neck MCQ With Explanation - 5 PDFDocumento5 páginasHead Neck MCQ With Explanation - 5 PDFMohamed GhabrunAinda não há avaliações
- CD PD 2.1 NECK 2017 Bates Outline PDFDocumento3 páginasCD PD 2.1 NECK 2017 Bates Outline PDFGiaFelicianoAinda não há avaliações
- Cordus Sacrus Eng - User ManualDocumento64 páginasCordus Sacrus Eng - User ManualRajesh JayakumarAinda não há avaliações
- MagnetoterapieDocumento10 páginasMagnetoterapieHelena PatraAinda não há avaliações
- CHS Physical Assessment GuideDocumento4 páginasCHS Physical Assessment GuideJosal SinonAinda não há avaliações
- Immersion Physical Exam Final - ChecklistDocumento2 páginasImmersion Physical Exam Final - ChecklistElizalde HusbandAinda não há avaliações
- A Randomized Controlled Trial of Exercise and Manipulative Therapy For Cervicogenic HeadacheDocumento9 páginasA Randomized Controlled Trial of Exercise and Manipulative Therapy For Cervicogenic Headachepaulina_810Ainda não há avaliações