Escolar Documentos
Profissional Documentos
Cultura Documentos
Testicular Cancer
Enviado por
Pro fatherDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Testicular Cancer
Enviado por
Pro fatherDireitos autorais:
Formatos disponíveis
Testicular Cancer
Plan
Defining the subject and its Epidemiology
The Classification and Investigations
The Treatment
What is it?
Primary Germ Cell Tumors of testis arising by malignant
transformation of primordial germ cells constitute 95% of
testicular neoplasms.
If GCTs arise from an extra-gonadal site: The mediastinum,
retro peritoneum, and very rarely, the pineal gland.
It is Notable for:
- 1) young age of afflicted patients.
- 2) Totipotent capacity for differentiation of the tumor cells
- 3) its curability.
Approximately, 95% of newly diagnosed patients are cured
Experience in the management of GCTs leads to improved
outcome.
Epidemiology
In 2010,
8480 new cases of testicular GCT were
diagnosed, and only 350 men were died in US
Ages 20-40 years old
Testicular mass > 50 years old regarded as
lymphoma untill proven otherwise
GCT is 4-5 times more common in whites than in
african blacks in US.
Testicular cancer
- Most common malignancy in men in the 15-35
year age group and evokes special interest
- One of most curable solid neoplasm
Serves as a paradigm for multimodal treatment
- Dramatic improvement in survival:
Effective diagnostic techniques
Tumour markers
Effective multidrug chemotherapeutic regimens
Modification of surgical technique
Classification of Testicular Tumours
Germ Cell Tumours
- Seminoma
Classic
Atypical
Spermatocytic
- Nonseminomatous
Embryonal carcinoma
Teratoma
Mature
Immature
Choriocarcinoma
Yolk sac tumor
CLASSIFICATION
I. Primary Neoplasms of Testis.
A. Germ Cell Tumor.
B.
Non-Germ Cell Tumor .
II.
Secondary Neoplasms.
III.
Paratesticular Tumors.
Germ cell tumors
1. Seminomas - 40%
(a) Classic Typical Seminoma
(b) Anaplastic Seminoma
(c) Spermatocytic Seminoma
2. Embryonal Carcinoma - 20 - 25%
3. Teratoma - 25 - 35%
(a) Mature
(b) Immature
4. Choriocarcinoma - 1%
5. Yolk Sac Tumour
Sex cord/ gonadal stromal tumors ( 5 to
10% )
1. Specialized gonadal stromal tumor
(a)
Leydig cell tumor
(b)
sertoli cell tumor
2. Gonadoblastoma
3. Miscellaneous Neoplasms
(a)
Carcinoid tumor
(b)
Tumors of ovarian epithelial sub
types
II. SECONDARY NEOPLASMS OF TESTIS
A.
Reticuloendothelial Neoplasms
B.
Metastases
III.
PARATESTICULAR NEOPLASMS
A.
Adenomatoid
B.
Cystadenoma of Epididymis
C.
Desmoplastic small round cell tumor
D.
Mesothelioma
E.
Melanotic neuroectodermal
Testicular cancer has become one of the most
curable cancers in US because of advances in
medical and surgical therapy
Cisplatin-based chemotherapy regimens have
improved the response rates for testis cancer
Examination
Detailed evaluation of neck, chest and abdominal
contents.
- Testicular tumors often have a palpable parenchymal testis
mass
Can be better appreciated if compared with contralateral normal
testicle.
- Needs to differentiate between
intraparenchymal testis masses often malignant
extraparenchymal testicular masses often benign.
- Scrotal ultrasound can distinguish intrinsic from extrinsic
testicular lesions with a high degree of accuracy and can
detect intratesticular lesions as small as 1 to 2 mm in
diameter.
Examination:
High-resolution CT scan of the abdomen,
pelvis and chest x-ray.
Regional metases first appear in the
retroperitoneal lymph nodes
CT to evaluate retroperitoneum, negative
results, as evidenced by a retroperitoneal
relapse rate of 20% to 25% in men, with
clinical stage I disease who do not undergo
retroperitoneal lymph node dissection RPLND
Labs
Serum marker alpha fetoprotein
Sb subunit of human chorionic gonadotropin
(Beta-HCG)
Lactate dehydrogenase
The differences between them:
- LDH is elevated in 80% to 85% of men with
nonseminomatous GCTs.
- In contrast, serum B-HCG is elevated in fewer than
20% of testicular seminomas
- AFP is not elevated in pure seminomas.
Neither serum B-HCG nor AFP alone or in
combination is sufficiently sensitive or specific
to establish the diagnosis of testicular cancer
in the absence of histologic confirmation.
Serum LDH concentrations are elevated in
30% to 80% of men with pure seminoma and
In 60% of those with nonseminomatous
tumors.
LDH is a less sensitive and less specific tumor
marker than B-HCG or AFP for men with
nonseminomatous GCTs
- But it may be the only marker that is elevated in
seminomas.
Significantly elevated serum LDH has
independent prognostic value in men with
advanced seminoma.
Radical inguinal orchiectomy with high ligation of
the spermatic cord near the internal inguinal ring
is performed to permit histologic evaluation of:
- primary tumor and provision of local tumor control.
- Note: Scrotal violation through scrotal incision or an
attempt to biopsy the testicle must be avoided
because of concern for changing the lymphatic
channels available to the testis tumor and potential
poorer outcome.
Serum half-lives of HCG and AFP are 18-36 hours and 5-7 days.
- Testicular cancer produces any of these serum markers
- Following progressive change after radical orchiectomy is an important
consideration in determining the adequacy of therapy.
Determination of histologic subtype of the testis cancer
Several parameters may identify patients at high risk for metastasis
to the retroperitoneum
- Despite absence of lymphadenopathy on the staging CT scan
- Nonseminomatous germ cell tumours, those factors include the
following:
1- Vascular lymph invasion
2- Primary tumor (T) Stage T2-T3
3- Embryonal carcinoma component greater than 40% of total tumor volume
Treatment
Patients with these risk factors who have no bulky
retroperitoneal lymphadenopathy
- Have normal tumor markers after radical orchiectomy
maybe candidates for RPLND.
Principles underlying modern surgical treatment of
testicular GCT
- based on stepwise predictable metastatic pattern of these
tumours
- Notable exception of choriocarcinoma
- RPLND is only reliable method to identify nodal
micrometases
- It is gold standard for providing accurate pathologic staging
of retroperitoneum
Both the number and size of involved
retroperitoneal lymph nodes have prognostic
importance
Surgical therapy for metastatic testicular
cancer has evolved
- The full bilateral RPLND used in the past evolved
first to a template-type Dissection
- Then to a nerve-sparing modification with a
unilateral template
RPLN
Surgical template for modified, left-sided (A)
and right-sided (B) retroperitoneal lymph
node dissection
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Neurological Paraneoplastic Syndromes: An OverviewDocumento13 páginasNeurological Paraneoplastic Syndromes: An OverviewPro father100% (1)
- Heart DefectsDocumento20 páginasHeart DefectsPro fatherAinda não há avaliações
- Clinical Case DiarrheaDocumento49 páginasClinical Case DiarrheaPro fatherAinda não há avaliações
- Abdominal PainDocumento38 páginasAbdominal PainPro fatherAinda não há avaliações
- Cervical CancerDocumento36 páginasCervical CancerPro fatherAinda não há avaliações
- Urinary Tract InfectionsDocumento18 páginasUrinary Tract InfectionsPro fatherAinda não há avaliações
- CIN & Cervical ScreeningDocumento51 páginasCIN & Cervical ScreeningPro fatherAinda não há avaliações
- Cumming - Otolaryngology - EpistaxisDocumento9 páginasCumming - Otolaryngology - EpistaxisPro fatherAinda não há avaliações
- Clinical Case On JaundiceDocumento43 páginasClinical Case On JaundicePro fatherAinda não há avaliações
- Peptic Ucler DiseaseDocumento2 páginasPeptic Ucler DiseasePro father100% (1)
- ECG LeadsDocumento13 páginasECG LeadsPro fatherAinda não há avaliações
- GI Bacterial InfectionsDocumento2 páginasGI Bacterial InfectionsPro fatherAinda não há avaliações
- Groundhog DayDocumento11 páginasGroundhog DayPro fatherAinda não há avaliações
- FMRIDocumento10 páginasFMRIPro fatherAinda não há avaliações
- Skull DevelopmentDocumento15 páginasSkull DevelopmentPro fatherAinda não há avaliações
- Apoptosis & NecrosisDocumento12 páginasApoptosis & NecrosisPro fatherAinda não há avaliações
- Cholinergic and Noradrenergic Neurons: Key Components of the Diffuse Modulatory SystemDocumento11 páginasCholinergic and Noradrenergic Neurons: Key Components of the Diffuse Modulatory SystemPro fatherAinda não há avaliações
- Neuroglia: Non-Neuronal Cells of The Nervous SystemDocumento18 páginasNeuroglia: Non-Neuronal Cells of The Nervous SystemPro fatherAinda não há avaliações
- Heart DefectsDocumento20 páginasHeart DefectsPro fatherAinda não há avaliações
- Billirubin MetabolismDocumento37 páginasBillirubin MetabolismPro father100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Entrepreneurship Project On Jam, Jelly & PicklesDocumento24 páginasEntrepreneurship Project On Jam, Jelly & Picklesashish karshinkarAinda não há avaliações
- Cs8791 Cloud Computing Unit2 NotesDocumento37 páginasCs8791 Cloud Computing Unit2 NotesTeju MelapattuAinda não há avaliações
- LSUBL6432ADocumento4 páginasLSUBL6432ATotoxaHCAinda não há avaliações
- Apollo TyresDocumento78 páginasApollo TyresADITYA33% (3)
- 3D Area Clearance Strategies for Roughing ComponentsDocumento6 páginas3D Area Clearance Strategies for Roughing ComponentsMohamedHassanAinda não há avaliações
- Abdomen - FRCEM SuccessDocumento275 páginasAbdomen - FRCEM SuccessAbin ThomasAinda não há avaliações
- Proceedings of The 16 TH WLCDocumento640 páginasProceedings of The 16 TH WLCSabrinaAinda não há avaliações
- De Thi HSG Tinh Binh PhuocDocumento9 páginasDe Thi HSG Tinh Binh PhuocDat Do TienAinda não há avaliações
- Taking Back SundayDocumento9 páginasTaking Back SundayBlack CrowAinda não há avaliações
- VivsayamDocumento87 páginasVivsayamvalarumsakthi100% (2)
- DR-M260 User Manual ENDocumento87 páginasDR-M260 User Manual ENMasa NourAinda não há avaliações
- Liquid Out, Temperature 25.5 °C Tube: M/gs P / WDocumento7 páginasLiquid Out, Temperature 25.5 °C Tube: M/gs P / WGianra RadityaAinda não há avaliações
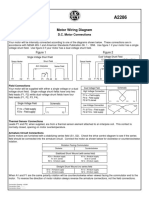
- Motor Wiring Diagram: D.C. Motor ConnectionsDocumento1 páginaMotor Wiring Diagram: D.C. Motor Connectionsczds6594Ainda não há avaliações
- VT6050 VT6010 QuickGuide ENDocumento19 páginasVT6050 VT6010 QuickGuide ENPriyank KumarAinda não há avaliações
- Handouts For TLG 3 1Documento5 páginasHandouts For TLG 3 1Daniela CapisnonAinda não há avaliações
- IEEE T&D Insulators 101 Design CriteriaDocumento84 páginasIEEE T&D Insulators 101 Design Criteriasachin HUAinda não há avaliações
- DENSO COMMON RAIL INJECTOR REPAIR GUIDEDocumento22 páginasDENSO COMMON RAIL INJECTOR REPAIR GUIDEMarcoAinda não há avaliações
- The Impact of Employees' Commitment Towards Food Safety at Ayana Resort, BaliDocumento58 páginasThe Impact of Employees' Commitment Towards Food Safety at Ayana Resort, Balirachelle agathaAinda não há avaliações
- Panasonic 2012 PDP Troubleshooting Guide ST50 ST Series (TM)Documento39 páginasPanasonic 2012 PDP Troubleshooting Guide ST50 ST Series (TM)Gordon Elder100% (5)
- Oral Nutrition Support NotesDocumento28 páginasOral Nutrition Support Notesleemon.mary.alipao8695Ainda não há avaliações
- Pharmacokinetics and Drug EffectsDocumento11 páginasPharmacokinetics and Drug Effectsmanilyn dacoAinda não há avaliações
- 07 Raction KineticsDocumento43 páginas07 Raction KineticsestefanoveiraAinda não há avaliações
- Casio AP-80R Service ManualDocumento41 páginasCasio AP-80R Service ManualEngkiong Go100% (1)
- (Razavi) Design of Analog Cmos Integrated CircuitsDocumento21 páginas(Razavi) Design of Analog Cmos Integrated CircuitsNiveditha Nivi100% (1)
- Current Relays Under Current CSG140Documento2 páginasCurrent Relays Under Current CSG140Abdul BasitAinda não há avaliações
- What Is DSP BuilderDocumento3 páginasWhat Is DSP BuilderĐỗ ToànAinda não há avaliações
- IS 4991 (1968) - Criteria For Blast Resistant Design of Structures For Explosions Above Ground-TableDocumento1 páginaIS 4991 (1968) - Criteria For Blast Resistant Design of Structures For Explosions Above Ground-TableRenieAinda não há avaliações
- Smart Grid Standards GuideDocumento11 páginasSmart Grid Standards GuideKeyboardMan19600% (1)
- Final Decision W - Cover Letter, 7-14-22Documento19 páginasFinal Decision W - Cover Letter, 7-14-22Helen BennettAinda não há avaliações
- Embankment PDFDocumento5 páginasEmbankment PDFTin Win HtutAinda não há avaliações