Escolar Documentos
Profissional Documentos
Cultura Documentos
Kuliah Enzyme Replacement Therapy 2012 Palangkaraya
Enviado por
Faridah Yuwono 280 notas0% acharam este documento útil (0 voto)
27 visualizações68 páginasmodul neurosains
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPTX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentomodul neurosains
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
27 visualizações68 páginasKuliah Enzyme Replacement Therapy 2012 Palangkaraya
Enviado por
Faridah Yuwono 28modul neurosains
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
Você está na página 1de 68
Yoga Devaera, Damayanti Rusli Sjarif
Div Pediatric Nutrition and Metabolic Diseases
Dept of Child Health FKUI/RSCM
Jakarta - Indonesia
After the lecture you should make a flowchart of how the
enzyme replacement therapy generated
Collect it tomorrow to your chief of the class
Assignment
Introduction
Enzyme replacement therapy
Summary
Outlines
They are looking for the answers to three basic
questions:
Is there a disease?
What causes it?
Can we prevent, treat, or cure it?
How do scientists investigate diseases?
Is there a disease ?
Whats wrong with this child?
Splenomegaly
In 1882, the French
medical student
Phillipe Charles Ernest
Gaucher described a
32-year old woman
whose spleen was
very enlarged.
Gaucher cells
A postmortem exam
revealed that spleen
infiltrated by cells, which
typically are large, pale,
polyhedral shaped cells
possessing a single,
relatively small,
eccentrically located
nucleus
Phillipe Charles Ernest Gaucher
Gaucher disease
Did people with Gaucher disease exist before
1882 ?
Yes, they did. But because a set of symptoms wasn't
identified with the condition, "Gaucher disease" as a
disease diagnosis did not exist.
Question 1
What causes it?
What Causes It?
In 1934, the French
chemist A. Aghion
discovered the
chemical cause of the
enlarged spleens and
liver: a buildup of a
lipid (fatty substance)
called
"glucocerebroside."
did people with Gaucher disease make too much of
the lipid for their bodies to handle?
Or did their bodies not break it down and dispose of
it?
Why there was too much lipid in
Gaucher cell ?
The answer to this question came during the
early 1960s, when Dr. Roscoe Brady's group
showed that
people with Gaucher disease made the lipid normally
but did not make enough of the enzyme
"glucocerebrosidase" to break it down and clear it out
of the body.
Development of a Gaucher cell
Gauchers disease is resulting from either
severely decreased functioning
or a complete lack of lysosomal acid -glucosidase or
glucocerebrosidase
Causes?
A single mutation in the gene coding for GCase can result
in partial (60-70%) or complete lack of enzyme activity
(Lieberman et al. 2007).
In affected cells, glucosylceramide accumulates and is
difficult to remove (glucosylceramide forms deposits
within macrophages called Lewy bodies that these cells
can't break down)
Buildup of glucosylceramide within macrophages can lead
to simultaneous enlargement of the spleen and liver,
abnormal bone turnover, and diseases of the central
nervous system in more severe cases (Lieberman et al.
2007).
Next findings
In 1967, Brady's group developed a convenient
diagnostic test for Gaucher disease which works
by measuring the activity of the enzyme
glucocerebrosidase in white blood cells.
The amount of enzyme directly relates to how
severe a case of Gaucher disease
The enzyme activity is also one way that may help
to distinguish the three types of Gaucher disease
described in this chart.
Enzyme activity
The Three Types of Gaucher Disease
Type 1 Type 2 Type 3
Whom it Strikes young adults /
adults
infants children/young
adults
Distinguishing
symptom
no nervous
system
problems
early nervous
system
problems
later onset of
nervous
system
problems
Effects of disease varies from
mild to
severe
dies in infancy becomes
severe
Glucocerebrosidase
Activity
some activity
but much
less than
normal
very little
activity
little activity
"Why do some people make too little enzyme?"
The answer to this
question came in
1987, when the first
gene mutation that
causes Gaucher
disease was
discovered by Dr. Shoji
Tsuji and coworkers.
chromosome 1
How Gaucher disease is passed on ?
Autosomal recessive
In the early 1970s, Dr. Brady's group devised
an enzymatic test based on the enzyme's activity to
tell people if they were carriers or not, and
a procedure for prenatal diagnosis.
These tests give people information about their
genetic status so that they can prepare for the
future.
Enzymatic based diagnosis
Can We Prevent, Treat, or
Cure It?
The third question that medical researchers try to
answer is the most important, and often depends
on the answer to the question what the cause of
it ?
To be truly successful, a treatment would have to
address the cause of the disease, not just the
symptoms.
For Gaucher disease, physicians initially attempted to
address the symptoms that accompany the disease.
They removed enlarged spleens, and performed liver
transplants, blood transfusions, and orthopedic
procedures.
Only bone marrow transplantation for people with Type I
Gaucher disease was sometimes successful.
mutation in gene coding enzyme
mutated enzyme
loss of
enzyme activity
accumulation of substrate
cell dysfunction /
biochemical and pathological change
clinical symptoms
The Pathophysiology of IEMs
The Principle of Treatment
gene mutation
mutated lysosome enzyme
loss of
enzyme activity
accumulation of substrate
cell dysfunction /
biochemical and pathological change
clinical symptoms
modification of
mutated protein
Chemical
Chaperone
inhibition of
substrate synthesis
Substrate
Deprivation
supplementation
of enzyme protein
ERT
BMT
Gene Therapy
ERT
In 1966, Dr. Roscoe Brady suggested a therapy for
Gaucher disease based on replacing the enzyme.
Using human placentas, Dr. Peter Pentchev of Dr.
Brady's team isolated a tiny sample of purified
glucocerebrosidase.
Enzyme Replacement Therapy
In 1973, Brady put that enzyme into two splenectomised
patients with Gaucher disease.
The first patient was a 15 year old boy with Type 3 Gauchers
disease.
a liver biopsy was obtained, the enzyme at u/kg/bw (unit
per kilo of bodyweight) was given and two days later
performed another liver biopsy a 26% reduction of the
accumulation of glucocerebroside in the liver biopsy.
The second patient also showed a 26% decrease.
The third patient received 2 u/kg/bw but the reduction was
only 8%
Development ERT
A large-scale purification method was completed in 1977.
The enzyme had to be treated with an alcohol to make it stick to
the purifying columns.
But this preparation of the enzyme produced inconsistent
results during clinical trials.
No reduction of hepatic (liver) glucocerebroside occurred in 4 out
7 patients who received this preparation
The alcohol had removed a lipid (fat) that activates the
enzyme and targets it to the affected cells, called
macrophages.
Development ERT
The problem was
the glucocerebrosidase was not going into the
macrophages, the cells in the liver, spleen and bone
marrow
that accumulate glucocerebroside: 95% of the infused
enzyme was going to other cells, primarily hepatocytes
in the liver, and being wasted.
Dr. Brady's challenge was now to get the purified
enzyme into the targeted cells.
Development ERT
John Barranger, Clifford Steer and Scott Furbish removed
oligosaccharides from the enzyme so that the mannose (a
sugar at the end of the sugar side chains) would attach to
the macrophage.
Modified Enzyme
In the first clinical trial with macrophage-targeted
glucocerebrosidase, eight people with Gaucher disease
received a fixed dose of the modified enzyme.
Only the smallest one - a child - experienced beneficial
effects. He was given 13 u/kg/bw every week.His
hemoglobin and platelet counts increased; the size of
his spleen and liver decreased; and the damage to his
bones lessened.
Then deliberately stopped the enzyme infusions and
his haemoglobin and platelets gradually decreased to
pre-infusion values.
Development ERT
When re-instated his enzyme infusions at 30 u/kg/bw, his
blood counts rose to normal range, there was a reduction in
the size of his spleen and liver and the damage to his bones
improved.
The other seven people were adults and had not received
enough of the enzyme to improve their condition.
It was at this point that Henri Termeer (now President
and Chief Executive Officer of Genzyme Corporation)
learned about the work.
Henri raised 10 million dollars to produce enough enzyme
for a clinical efficacy trial.
Brady's team then carried out a dose response study and
elected to give patients 60 u/kg/bw every two weeks. In
this clinical efficacy trial, all 12 patients improved.
All of these people had strikingly good clinical responses
within a few months. For example, their height and
weight increased; their anemia improved; their liver and
spleen sizes decreased; and their bone damage lessened.
Dose Response Study
Hemoglobin Chart
Before and after X-
Rays
Macrophage-targeted glucocerebrosidase was
approved as a specific treatment for Gaucher
disease by the Federal Drug Administration on
April 5, 1991.
Enzyme replacement therapy worked. Ceredase
worked and the recombinant enzyme Cerezyme is
just as good.
Enzyme replacement therapy is an effective
treatment for most people with Type 1 Gaucher
disease.
FDA approval
FDA approval
ERT for Gaucher Diseases
Pretreatment
Female; Age 8 Years, 8 Months
Post-treatment
Female; Age 10 Years, 10 Months
Gauchers patient Response to Enzyme Therapy
Courtesy of NW Barton. Developmental and Metabolic Neurology Branch of the NINDS.
Therapeutic Goals and Monitoring for Type 1
Gaucher Disease
Recombinant Enzyme Disorder Comment
Imiglucerase
Nonneuronopathic (type 1)
Gaucher disease
reported to reduce hepatosplenomegaly,
improve anemia and thrombocytopenia, and
reduce episodes of pain crises in these
patients.Because the recombinant enzyme does
not cross the blood-brain barrier, it is not
effective in type 2 Gaucher disease patients
with severe CNS abnormalities
Alpha-galactosidase
(2003)
Fabry disease
Improvement in pain and gastrointestinal
symptoms has been reported, but long-term
studies are required for evaluating its efficacy
with respect to life-threatening complication
Laronidase (2003) MPS I
reported improvements in hepatosplenomegaly
and respiratory disease and showing a decrease
in urinary glycosaminoglycan excretion.
Hematopoietic Stem Cell Transplantation (HCT)
is currently the mainstay of therapy for MPS I
Arylsulfatase B (2005)
MPS VI (Maroteaux-Lamy
syndrome)
associated with improvements in
hepatosplenomegaly, joint movement,
cardiopulmonary function, and pain as well as
reduced excretion of urinary
glycosaminoglycans
Alglucosidase alpha Infantile Pompe disease
A portion of infants who are diagnosed and
treated with ERT before 6 months of age had
improved survival and quality of life compared
with the observed natural history of the
disease, yet, for unknown reasons, a subset of
the treated cohort did not show effects from
ERT
Idursulfase
MPS II (Hunter
syndrome)
Clinical trials showed improvement in
cardiopulmonary disease and
hepatosplenomegaly and decreased excretion of
urinary glycosaminoglycans
ERT in Pompe diseases
Pompe: patient response to enzyme therapy
MPS 1: Improved Joint Range of Motion
Pretreatment
Posttreatment 26weeks
Mean Changes in the Restriction of Range of Motion in
Patients with Mucopolysaccharidosis I during -l-
Iduronidase Therapy
ERT has little effect on the brain, skeletal tissue, and
valvular heart disease in LSDs.
ERT treats only the symptoms and not the underlying
disease
Lifelong frequent infusions (weekly to monthly depending
on the protocol)
The estimated cost of ERT is between $90,000 to $565,000
(US), depending on the disease (therapy) and patient size.
Intravenous infusions of GCase are administered
weekly and it can cost a patient from $100,000 to
$750,000 per year (Sawkar et. al, 2002).
Infusion reactions including fatal anaphylaxis have been
reported
Limitations of enzyme replacement therapy
Other therapy options are
highly desirable !!!!
K, female, 8 years old
Suspected Fabry since 3 years old
Diagnosed Fabry at 8 years old
ERT cost
Rp 180.000.000,-/month
Lifelong
Donation ?
Fabry Diseases : Waiting for ERT
Fabry disease progression
Clinical staging of Fabry disease in the kidney. (Reproduced
with permission from Branton MH, et al. Medicine.
2002;81:122-38.)
F, 3 years old boy diagnosed as MPS IVA (Morquio
Syndrome)
No ERT available yet
Trial of ERT beginning 2012 in Taiwan, refused because of
nationality
MPS IVA : Waiting for ERT (trial)
Thank you
Gaucher disease - massive splenomegaly
splenomegaly
The enlarged cells (now
called "Gaucher cells")
and spleen became signs
of the disease.
Gaucher's description of
the them enabled other
physicians to diagnose
people with Gaucher
disease, and introduce
the term into medical
literature
Lysosomal glucosylceramide accumulation in Gaucher
stabilizes -synuclein oligomers -synuclein inhibits
lysosomal trafficking of glucocerebrosidase in
synucleinopathies
Você também pode gostar
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Drugs Used in Gastrointestinal Diseases FinalDocumento30 páginasDrugs Used in Gastrointestinal Diseases FinalFaridah Yuwono 28Ainda não há avaliações
- From Philo To Plotinus AftermanDocumento21 páginasFrom Philo To Plotinus AftermanRaphael888Ainda não há avaliações
- Methods of Recording Retruded Contact Position in Dentate PatientsDocumento15 páginasMethods of Recording Retruded Contact Position in Dentate PatientsYossr MokhtarAinda não há avaliações
- Chapter 3 - Organization Structure & CultureDocumento63 páginasChapter 3 - Organization Structure & CultureDr. Shuva GhoshAinda não há avaliações
- DC 7 BrochureDocumento4 páginasDC 7 Brochures_a_r_r_yAinda não há avaliações
- Sistem Informasi Dan Administrasi Pemasaran Pada PT - Kaltengpos Press Berbasis WebDocumento13 páginasSistem Informasi Dan Administrasi Pemasaran Pada PT - Kaltengpos Press Berbasis WebFaridah Yuwono 28Ainda não há avaliações
- LipidDocumento38 páginasLipidFaridah Yuwono 28Ainda não há avaliações
- Lecture 3 DNA RNA Gen Structure Ade FKUI 2012Documento44 páginasLecture 3 DNA RNA Gen Structure Ade FKUI 2012Faridah Yuwono 28Ainda não há avaliações
- Neuro ImagingDocumento41 páginasNeuro ImagingFaridah Yuwono 28Ainda não há avaliações
- Gene Transcription 1Documento18 páginasGene Transcription 1Faridah Yuwono 28Ainda não há avaliações
- SPECIAL SENSES HearequismltasteDocumento22 páginasSPECIAL SENSES HearequismltasteFaridah Yuwono 28Ainda não há avaliações
- Human Reproductive System and Human Development: Deswaty FurqonitaDocumento33 páginasHuman Reproductive System and Human Development: Deswaty FurqonitaFaridah Yuwono 28Ainda não há avaliações
- Antiangina and Hipolipidemic AgentsDocumento83 páginasAntiangina and Hipolipidemic AgentsFaridah Yuwono 28Ainda não há avaliações
- Cardiovasc.-Nutr Therapy - Univ PlkrayaDocumento67 páginasCardiovasc.-Nutr Therapy - Univ PlkrayaFaridah Yuwono 28Ainda não há avaliações
- Community Medicine Department Faculty of Medicine University of Indonesia Setyawati Budiningsih, Retno Asti Werdhani Nuri Purwito Adi April 4th 2012Documento60 páginasCommunity Medicine Department Faculty of Medicine University of Indonesia Setyawati Budiningsih, Retno Asti Werdhani Nuri Purwito Adi April 4th 2012Faridah Yuwono 28Ainda não há avaliações
- Gods Omnipresence in The World On Possible MeaninDocumento20 páginasGods Omnipresence in The World On Possible MeaninJoan Amanci Casas MuñozAinda não há avaliações
- PyhookDocumento23 páginasPyhooktuan tuanAinda não há avaliações
- Aleksandrov I Dis 1-50.ru - enDocumento50 páginasAleksandrov I Dis 1-50.ru - enNabeel AdilAinda não há avaliações
- Harper Independent Distributor Tri FoldDocumento2 páginasHarper Independent Distributor Tri FoldYipper ShnipperAinda não há avaliações
- Aptitude Number System PDFDocumento5 páginasAptitude Number System PDFharieswaranAinda não há avaliações
- Career Essay 1Documento2 páginasCareer Essay 1api-572592063Ainda não há avaliações
- Corrosion Fatigue Phenomena Learned From Failure AnalysisDocumento10 páginasCorrosion Fatigue Phenomena Learned From Failure AnalysisDavid Jose Velandia MunozAinda não há avaliações
- 3 Carbohydrates' StructureDocumento33 páginas3 Carbohydrates' StructureDilan TeodoroAinda não há avaliações
- Carob-Tree As CO2 Sink in The Carbon MarketDocumento5 páginasCarob-Tree As CO2 Sink in The Carbon MarketFayssal KartobiAinda não há avaliações
- Technical Bulletin LXL: No. Subject Release DateDocumento8 páginasTechnical Bulletin LXL: No. Subject Release DateTrunggana AbdulAinda não há avaliações
- ME Eng 8 Q1 0101 - SG - African History and LiteratureDocumento13 páginasME Eng 8 Q1 0101 - SG - African History and Literaturerosary bersanoAinda não há avaliações
- BMOM5203 Full Version Study GuideDocumento57 páginasBMOM5203 Full Version Study GuideZaid ChelseaAinda não há avaliações
- Law of EvidenceDocumento14 páginasLaw of EvidenceIsha ChavanAinda não há avaliações
- Chapter 13 Exercises With AnswerDocumento5 páginasChapter 13 Exercises With AnswerTabitha HowardAinda não há avaliações
- The Doshas in A Nutshell - : Vata Pitta KaphaDocumento1 páginaThe Doshas in A Nutshell - : Vata Pitta KaphaCheryl LynnAinda não há avaliações
- All You Need To Know About Egg YolkDocumento7 páginasAll You Need To Know About Egg YolkGolden Era BookwormAinda não há avaliações
- SMR 13 Math 201 SyllabusDocumento2 páginasSMR 13 Math 201 SyllabusFurkan ErisAinda não há avaliações
- Lesson PlanDocumento2 páginasLesson Plannicole rigonAinda não há avaliações
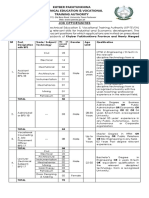
- KP Tevta Advertisement 16-09-2019Documento4 páginasKP Tevta Advertisement 16-09-2019Ishaq AminAinda não há avaliações
- Dtu Placement BrouchureDocumento25 páginasDtu Placement BrouchureAbhishek KumarAinda não há avaliações
- Chapter 1 To 5 For Printing.2Documento86 páginasChapter 1 To 5 For Printing.2Senku ishigamiAinda não há avaliações
- Soosan Crane Training: (Principles)Documento119 páginasSoosan Crane Training: (Principles)Boumediene CHIKHAOUIAinda não há avaliações
- Laboratory Manual (CIV 210) Engineering Surveying (2018-19) (For Private Circulation Only)Documento76 páginasLaboratory Manual (CIV 210) Engineering Surveying (2018-19) (For Private Circulation Only)gyanendraAinda não há avaliações
- DPSD ProjectDocumento30 páginasDPSD ProjectSri NidhiAinda não há avaliações
- 8.ZXSDR B8200 (L200) Principle and Hardware Structure Training Manual-45Documento45 páginas8.ZXSDR B8200 (L200) Principle and Hardware Structure Training Manual-45mehdi_mehdiAinda não há avaliações
- On Derridean Différance - UsiefDocumento16 páginasOn Derridean Différance - UsiefS JEROME 2070505Ainda não há avaliações