Escolar Documentos
Profissional Documentos
Cultura Documentos
Nepro Pharmacology
Enviado por
guestarDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Nepro Pharmacology
Enviado por
guestarDireitos autorais:
Formatos disponíveis
NEPHRO
PHARMACOLOGY
Introduction
Kidney comprise only 0,5 %
BW,but receive 25 % CO
So,drugs can damage the
kidney,renal disease affects
responses to drugs
The recognition of DIRD is very
important because the resulting
ARF & CRF potentially
reversible & preventable
Subtopics
Drugs induced renal disease
(=DIRD)
Drugs presecibing in renal
disorders
Mechanisms of DIRD
1) Direct biochemical effect :
Heavy metals(Hg,Au,Fe,Pb)
Antimicrobial(Aminoglycosidea,
Cephalosporins,sulphonamides)
Contrast media(biliary)
analgesices(aspirin)
Solvents(CCL4,Ethylene Glycol)
2) Indirect biochemical effect :
Urisocurics urate
precipitation
Calciferol renal calcification
Diuretic/laxative tubular
damage
Sulphonamides crystallise in
UT
Anticoagulant haemorrage
into kidney
3) Immunological effect :
Penicilin,sulphonamides,isoniazid,
Rifampicin
Phenytoin,procainamide,
hydralazine
Au,penicillamine
A drugs renal disease,by >1
mechanisms(sulponamides)
Sites & Pathological types
of DIRD
1. Glomerular
2. Tubular
Damage proximal,medulla,distal
Obstruction
3. Other DIRD
1.Glomerular : large surface area
of glomerular
capillaries susceptible to
damage from circulation
immune complexes
Penicillamine :
glomerulonephritis proteinuria
nephrotic syndrome
Creatinie clearance (=CcR)
a measure of glomerular
filtration rate (=GFR)
Formula of Cockcroft & Gault :
CcR = (140 age ) x BW
72 x Cs
Notes : - Cs = serum creatinine
- Women = Man 15 %
2. Tubular
Tubular damage
200 L/day GF 1,5 L/day
urine renal tubular cells
expose more than other cells to
toxins
Proximal,medulla,distal tubular
Tubular obstruction
certain physico chemical
condition crystal can deposit
within tubular lumen
Tubular proximal toxicity
By acids
(salicylates,cephalosporins),
bases(aminoglycosides),heavy
metals and contrast media
Urinary excretion,of glucose,
phosphate,HCO3,amino acids
Medullary toxicity
NSAID >< local Pg ischaemia
analgesic nephropathy
Distal tubular toxicity
Under physico-chemical
conditions,crystal can deposit
within tubular lumen
Methotrexate(relative insoluble
at law Ph) can precipitate in
distal tubular when urine is acid
Nucleic acids(in leukemic cells)
breakdown by chemotherapy
insoluble urate will be precipitate
3. Other DIRD
Vasculitis by
sulphonamide,allopurinol,
isoniazid
Allergic Interstitial Nephritis by
panicillins,sulphonamides,
thiazides,allopurinol,phenytoin
SLE by
hydralazine,procainamide
ARF by
aminoglycosides,cisplatin
NS by penicillamine,Au,ceptopril
CRF by NSAID,amphotefricin-B
Functional impairment due to
impairment to dilute/concentrate
urine,potassium loss,acid-base
ambalance
Vulnerability factor to DIRD
1) High work-load of renal
function
2) Glomerural endothelial surface
area >
3) Capacity to concentrate of
drugs & nephrotoxins in lumen
4) Liability to immune injury
5) Accumulation of drugs &
metabolites(in renal
insufficiency)
Drugs may :
1. Exacerbate renal disease
2. Accumulate,due to failure of
renal excreation / changes in
protein binding
3. Be ineffective,e.g thiazide in
moderate/severe renal failure,
uricosurics
Problem:
RF patient must be treated with
neprotoxic dugs & largely
eliminated by the kidney
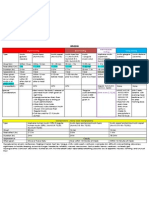
Drugs classification base
renal elimination
(A) Almost exclusively eliminated by
the kidney
drugs half life(T)
N S-RF
- Benzylpenicilline 0,5 8
- Ampicillin 1 14
- Acyclovir 2,5 20
- Gentamicin 2,5 50
- Sotalol 5 41
- Atenolol 6 100
- Tetracycline 8 75
T = half life
= The time for its concentrate
to halve,after absorption
and distribution of the drug
are complete
(B1) Almost entirely metabolized
drugs half life (T)
N S-RF
- Paracetamol 2 2
- Clindamycin 2 3
- Propranolol 3 3
- Rifampicin 3 3
- Lorazepam 15 15
- Doxycycline 18 18
- Notriptyline 30 30
- Warfarin 40 40
(B2) Drugs produce
pharmacologically active
metabolites(water-soluble)
renal elimination
In RF accumulate
e.g. - Acebutolol,hydralazine,
isosorbide
- Allopurinol,
carbamazepine
- Chordiazepoxide,
diazepam,clobazam,
flurazepam
- Metronidazole,5-FU
(C) Partly metabolized & partly
eliminated by the kidney
drugs Half life (T)
N S-RF
- Lincomycin 5 12
- Trimethoprim 10 25
- Amphetamine 12 24
- Chlorpropamide 36 280
- Digoxin 36 120
- Digitoxin 150 240
Dosing regimens in renal
impairment (general rule)
Group A/B2 :
Initial dose-normal/slightly
Maintenance dose or interval
dose
Group B1 :
Initial dose-normal or in
advanced-RD,Hypoproteinemia,
drugs with highly protein binding
Group C :
Initial dose-normal
Maintenance dose/interval dose
will be modified
Drugs Group A or B
regimens in CRF
- DIN = DIo x 1/Q
- MDN = MDo x Q
Notes :
Q = Adjustment factor=PCcr/NCer
DIN = New Interval Dose
NCer = Normal Ccr
MDN = New Maintenance Dose
DIo = Old Interval Dose
PCcr = Patient Ccr
MDo = Old Maintenance Dose
- Alteration in renal function on
drug elimination depend on 2
factor :
1. Unchangee drug fraction
normally eliminated by the
kidney
2. Degree of renal insufficiency
- Estimation of Ccr remains the
guiding factor for dose regimen
design
If the metabolites are inactive &
non-toxic and the drug(group C)
obey first-order(linear)
kinetic,the principle of
adjustment factor are :
Qc = I [Fc (1- KF)]
- DIN = DIo x 1/Q
- MDN = MDo x Q
KF = PCcr/NCcr
Fc = Unchanged drug fraction
normally eliminated by the
kidney
Calculation Dose Regimen
by Using Half Life(T)
DF = T normal / T RF
DDRF = DDn x DF
DIRF = DIN / DF
DF = Drug Fraction
DD = Drug Dose
DI = Drud Interval
Drug prescribing guidelines
in RF
1. Use a drug in definite indications
2. Choose a drug with minimal
nephrotoxics effect
3. Use plasma level to adjust the
dose
4. Use recommended dosage
regimens for RF
5. Avoid prolonged courses of
potientially toxic drugs
6. Avoid potientially nephrotoxic
combination of drugs
7. Monitor the patient carefully for
clinical efficacy & evidence of
toxicity
Você também pode gostar
- Medicinal Chemistry of Drugs Affecting the Nervous SystemNo EverandMedicinal Chemistry of Drugs Affecting the Nervous SystemAinda não há avaliações
- NEPHROPHARMACOLOGYDocumento24 páginasNEPHROPHARMACOLOGYYogie Pratama RamliAinda não há avaliações
- Acute Kidney InjuryDocumento25 páginasAcute Kidney Injuryradhakishan.22phpp09Ainda não há avaliações
- K.23 Farmakologi (2) Pada Gagal GinjalDocumento52 páginasK.23 Farmakologi (2) Pada Gagal GinjalHernita FerliyaniAinda não há avaliações
- Antiaritmia: Frans D. Suyatna Modified by Sulistia 1010 Departemen Farmakologi & Terapeutik FKUIDocumento56 páginasAntiaritmia: Frans D. Suyatna Modified by Sulistia 1010 Departemen Farmakologi & Terapeutik FKUIJoshua ObrienAinda não há avaliações
- Antihypertensive AgentsDocumento33 páginasAntihypertensive AgentsJuwairia tariqAinda não há avaliações
- 8 BSC 2014 Sweeney B Individual Variability in Pharmacological PDFDocumento46 páginas8 BSC 2014 Sweeney B Individual Variability in Pharmacological PDFBogdan CarabasAinda não há avaliações
- Drugs and Kidney DiseasesDocumento46 páginasDrugs and Kidney Diseasesمرتضى محمد فاضل جرجوكAinda não há avaliações
- Cardiac ArrhythmiaDocumento101 páginasCardiac ArrhythmiaYuvraj ChauhanAinda não há avaliações
- Cardiology Pharmacology Review: Dhiren Patel, Pharmd, CdeDocumento74 páginasCardiology Pharmacology Review: Dhiren Patel, Pharmd, Cdeshannon_marrero_1Ainda não há avaliações
- Chemotherapy and Renal Andhepatic Insufficiency 2008Documento24 páginasChemotherapy and Renal Andhepatic Insufficiency 2008Vika RatuAinda não há avaliações
- Guidelines For Prescribing in Renal Failure: 37.1 General PrinciplesDocumento9 páginasGuidelines For Prescribing in Renal Failure: 37.1 General PrinciplesArshAinda não há avaliações
- Parasympathetic Nervous System: Uptake of CholineDocumento16 páginasParasympathetic Nervous System: Uptake of Cholinegksah711Ainda não há avaliações
- Antihypertensive Drugs - Classification and SynthesisDocumento14 páginasAntihypertensive Drugs - Classification and SynthesisCường NguyễnAinda não há avaliações
- Arrhythmias!Documento49 páginasArrhythmias!mospala285Ainda não há avaliações
- Adverse Drug Reactions and Drug InteractionsDocumento10 páginasAdverse Drug Reactions and Drug Interactions88AKKAinda não há avaliações
- FAQ - FinerenoneDocumento9 páginasFAQ - Finerenoneraea.dobsonAinda não há avaliações
- Drug Induced Liver Diseases (DILD) : M. DeepalakshmiDocumento22 páginasDrug Induced Liver Diseases (DILD) : M. DeepalakshmicrissAinda não há avaliações
- KIDNEY AND DRUGSDocumento17 páginasKIDNEY AND DRUGSapi-3761895Ainda não há avaliações
- Drugs & KidneyDocumento18 páginasDrugs & KidneyAamir MohammadAinda não há avaliações
- Dosage Adjustment of Cytotoxics in Renal ImpairmentDocumento24 páginasDosage Adjustment of Cytotoxics in Renal ImpairmenthamzaAinda não há avaliações
- Antiarrhythmic AgentsDocumento45 páginasAntiarrhythmic AgentsSoh Kae SiangAinda não há avaliações
- Angina Pharmacology YeahDocumento16 páginasAngina Pharmacology YeahMuhammad AfifuddinAinda não há avaliações
- Anti-Parkinsonism DrugDocumento15 páginasAnti-Parkinsonism Drugsaihjad pramaniAinda não há avaliações
- PharmacologyDocumento116 páginasPharmacologyvargheseAinda não há avaliações
- FlupentixolDocumento30 páginasFlupentixolAhmed AbedoAinda não há avaliações
- Phenelzine - Liver ToxicityDocumento8 páginasPhenelzine - Liver Toxicitydo leeAinda não há avaliações
- Antiarrhythmic DrugsDocumento17 páginasAntiarrhythmic DrugsTarek G MustafaAinda não há avaliações
- Drugs and Renal DiseasesDocumento31 páginasDrugs and Renal DiseasesStanley Tatenda MukonoAinda não há avaliações
- PARKINSONSDocumento82 páginasPARKINSONSCesarMatthewUlepMadriaAinda não há avaliações
- SympatholyticsDocumento46 páginasSympatholyticsHari Kamesh KiranAinda não há avaliações
- A.10. What Is The Mechanism of Action of Antihypertensive Drugs?Documento2 páginasA.10. What Is The Mechanism of Action of Antihypertensive Drugs?Albert Tesoro Silang Jr.Ainda não há avaliações
- Pharmacokinetic Interaction: DR - Datten Bangun MSC, SPFK & DR - Zulkarnain RangkutyDocumento39 páginasPharmacokinetic Interaction: DR - Datten Bangun MSC, SPFK & DR - Zulkarnain RangkutyCatherine ElizabetAinda não há avaliações
- June 2019 154points Ashraf-1Documento11 páginasJune 2019 154points Ashraf-1majid tariqAinda não há avaliações
- UntitledDocumento44 páginasUntitledTani BirlaAinda não há avaliações
- Icu ProtocolDocumento4 páginasIcu Protocolmehal guptaAinda não há avaliações
- Dept - Farmakologi & Terapeutik Fak - Kedokteran U S U Medan: Prof - Dr.H.Aznan Lelo PHD - SPFK DR - Datten Bangun MSC, SPFKDocumento62 páginasDept - Farmakologi & Terapeutik Fak - Kedokteran U S U Medan: Prof - Dr.H.Aznan Lelo PHD - SPFK DR - Datten Bangun MSC, SPFKAnonymous zZrGTONhAinda não há avaliações
- AntiemeticsDocumento37 páginasAntiemeticsAriel OlshevskyAinda não há avaliações
- Drugs and The Kidney: Continuing Medical EducationDocumento6 páginasDrugs and The Kidney: Continuing Medical EducationJANINE PASIONAinda não há avaliações
- Parkinson - S Disease Case PresentationDocumento39 páginasParkinson - S Disease Case PresentationAnonymous dpxYTE0% (1)
- Liver DiseaseDocumento17 páginasLiver DiseaseGANESH KUMAR JELLAAinda não há avaliações
- Pharmacology of Antianginal Drugs: Tri Widyawati M. IchwanDocumento43 páginasPharmacology of Antianginal Drugs: Tri Widyawati M. IchwanYohanna SinuhajiAinda não há avaliações
- MedSurg Medication Study Guide Test 1Documento12 páginasMedSurg Medication Study Guide Test 1Sarah PlunkettAinda não há avaliações
- Acute Renal Failure BDocumento60 páginasAcute Renal Failure BEzekiel moraraAinda não há avaliações
- Obat Antihypertensi: DR Med DR - Widharto PH, SPFK Farmakologi Dan Terapi Fak - Kedokteran UgmDocumento38 páginasObat Antihypertensi: DR Med DR - Widharto PH, SPFK Farmakologi Dan Terapi Fak - Kedokteran UgmNi Made Dwiki AndriyaniAinda não há avaliações
- CASESDocumento36 páginasCASESRoro RageyAinda não há avaliações
- ART Rugs and Nfusions: A. PolicyDocumento7 páginasART Rugs and Nfusions: A. PolicyZoelAinda não há avaliações
- Antiseizure: Medical University of Sofia, Faculty of Medicine Department of Pharmacology and ToxicologyDocumento29 páginasAntiseizure: Medical University of Sofia, Faculty of Medicine Department of Pharmacology and Toxicologybudirahmant0Ainda não há avaliações
- Principles of The Anaesthetic Management of Patient With Renal FailureDocumento18 páginasPrinciples of The Anaesthetic Management of Patient With Renal FailureAndrewBeckAinda não há avaliações
- Anaesthesia in CKD MAJUDocumento21 páginasAnaesthesia in CKD MAJUAnonymous BQM9271ZXAinda não há avaliações
- And Other Movement DisordersDocumento38 páginasAnd Other Movement DisordersshravaniAinda não há avaliações
- Molecules: Antiparkinson ProdrugsDocumento23 páginasMolecules: Antiparkinson ProdrugsShasha elshaAinda não há avaliações
- Pharmacology Notes: By: Khurram AbbasDocumento48 páginasPharmacology Notes: By: Khurram AbbasAsma AnjumAinda não há avaliações
- Antiarrhytmic Talk For ResidenDocumento90 páginasAntiarrhytmic Talk For ResidenMusa yohanaAinda não há avaliações
- Dacarbazine Monograph 1june2013 FormattedDocumento7 páginasDacarbazine Monograph 1june2013 FormattedRobert ChristevenAinda não há avaliações
- Lecture 22. Drugs Used in Renal and Urinary Tract DisordersDocumento38 páginasLecture 22. Drugs Used in Renal and Urinary Tract DisorderskrisnadewirahadiAinda não há avaliações
- Drug Interaction-SibyDocumento93 páginasDrug Interaction-SibyAswin DamodaranAinda não há avaliações
- Fpgee Test PracticeDocumento31 páginasFpgee Test Practiceapi-3830277100% (2)
- Non-Parkinsonian Movement DisordersNo EverandNon-Parkinsonian Movement DisordersDeborah A. HallAinda não há avaliações
- M80e - 7 10 07Documento36 páginasM80e - 7 10 07guestarAinda não há avaliações
- Anti-Anemia DrugsDocumento25 páginasAnti-Anemia DrugsAdrul FauzanAinda não há avaliações
- DiverticulosisDocumento8 páginasDiverticulosisguestarAinda não há avaliações
- Anti Virus Anti JamurDocumento53 páginasAnti Virus Anti JamurguestarAinda não há avaliações
- InsulinDocumento13 páginasInsulinguestarAinda não há avaliações
- Obat-Obat AnthelmintikDocumento46 páginasObat-Obat AnthelmintikguestarAinda não há avaliações
- Tym Pa No SclerosisDocumento6 páginasTym Pa No SclerosisguestarAinda não há avaliações
- Bullous MyringitisDocumento4 páginasBullous MyringitisguestarAinda não há avaliações
- OtosklerosisDocumento13 páginasOtosklerosisguestarAinda não há avaliações
- Acoustic NeuromaDocumento21 páginasAcoustic NeuromaguestarAinda não há avaliações
- Vestibular Neuritis: DR Ika Yuliartanti.,Sptht-Kl.,M.KesDocumento5 páginasVestibular Neuritis: DR Ika Yuliartanti.,Sptht-Kl.,M.KesguestarAinda não há avaliações
- 02 Vitamin ADocumento22 páginas02 Vitamin AguestarAinda não há avaliações
- Sclera: Dr. Bambang Susetio, SPMDocumento19 páginasSclera: Dr. Bambang Susetio, SPMmalim fairrulAinda não há avaliações
- UveaDocumento43 páginasUveaguestarAinda não há avaliações
- Unjani - RS Dustira Cimahi 2008Documento8 páginasUnjani - RS Dustira Cimahi 2008Agniya Ali FahmiAinda não há avaliações
- Vol 6 - Nervous System AgentsDocumento1.080 páginasVol 6 - Nervous System Agentsjoshigauta100% (3)
- Ενιαιοσ Τιμοκαταλογοσ 20140508 (Single Price)Documento656 páginasΕνιαιοσ Τιμοκαταλογοσ 20140508 (Single Price)Anuj MairhAinda não há avaliações
- 2008, Vol.92, Issues 5, Women's HealthDocumento312 páginas2008, Vol.92, Issues 5, Women's HealthHussain OudahAinda não há avaliações
- The Essentials of Pain ManagementDocumento46 páginasThe Essentials of Pain ManagementTaufik Akbar Faried LubisAinda não há avaliações
- Pharmacotherapy Handbook 9th Edition 2015-BAB KULITDocumento19 páginasPharmacotherapy Handbook 9th Edition 2015-BAB KULITCrista Resti StarillaAinda não há avaliações
- Apotex - Wikipedia, The Free EncyclopediaDocumento4 páginasApotex - Wikipedia, The Free EncyclopediaOluwafemi DagunduroAinda não há avaliações
- NRS 230 Pharmacology Week 1 Students - 11!22!11Documento110 páginasNRS 230 Pharmacology Week 1 Students - 11!22!11angieswensonAinda não há avaliações
- 2015 07 10 Pharma Distribution RomaniaDocumento2 páginas2015 07 10 Pharma Distribution RomaniaVanillaheroineAinda não há avaliações
- Insulin Chart 05032012 PDFDocumento1 páginaInsulin Chart 05032012 PDFTiffany CrittendenAinda não há avaliações
- List of Drugs For FinalsDocumento3 páginasList of Drugs For FinalsLena EmataAinda não há avaliações
- NAPLEX Calc PracticeDocumento10 páginasNAPLEX Calc PracticeYasmin Amr Nounou100% (2)
- Operation Management Facility Layout: Atharva Institute of Management StudiesDocumento4 páginasOperation Management Facility Layout: Atharva Institute of Management Studiesnika_001Ainda não há avaliações
- Oral Health & The Renal PatientDocumento2 páginasOral Health & The Renal PatientRahemin MalikAinda não há avaliações
- Kentucky: Medicare Advantage Cost Plans and DemonstrationsDocumento46 páginasKentucky: Medicare Advantage Cost Plans and Demonstrationsanon-76504Ainda não há avaliações
- Tablet Splitting - To Split or Not To SplitDocumento2 páginasTablet Splitting - To Split or Not To Splitcarramrod2Ainda não há avaliações
- Adee Lifesciences PCD Product SheetDocumento6 páginasAdee Lifesciences PCD Product Sheetrjskalu123 123Ainda não há avaliações
- Drug StudyDocumento3 páginasDrug StudyMarychen Cabunas100% (1)
- Drug StudyDocumento4 páginasDrug StudyHarold Dave IgcalinosAinda não há avaliações
- ChemoStabilityChart AtoK 14jan2014Documento42 páginasChemoStabilityChart AtoK 14jan2014nofiasaridAinda não há avaliações
- Daftar Obat DR - Sps DalamDocumento3 páginasDaftar Obat DR - Sps DalamKlinik Sosa Graha MedikaAinda não há avaliações
- Rectal SuppositoriesDocumento2 páginasRectal SuppositoriesAngel Leo M. ZuñigaAinda não há avaliações
- Odb CdiDocumento644 páginasOdb CdiPaul JagdharryAinda não há avaliações
- Critical AppraisalDocumento2 páginasCritical AppraisalHJ GAinda não há avaliações
- Drug ListDocumento9 páginasDrug ListsinghajitbAinda não há avaliações
- Barrier Isolator WikiDocumento2 páginasBarrier Isolator Wikiana_mondekarAinda não há avaliações
- Nexpro Uae FinalDocumento13 páginasNexpro Uae Finalamr ahmedAinda não há avaliações
- United State PharmacopeiaDocumento42 páginasUnited State PharmacopeiashamsAinda não há avaliações
- AugmentinDocumento7 páginasAugmentinHeba_Al_Khozae0% (1)
- MCQ On Cardiology IDocumento84 páginasMCQ On Cardiology IHarsh Oak50% (2)
- Generic Drug Suffix ChartDocumento19 páginasGeneric Drug Suffix ChartstarobinAinda não há avaliações