Escolar Documentos
Profissional Documentos
Cultura Documentos
Body Fluids
Enviado por
clarintaucha100%(1)100% acharam este documento útil (1 voto)
142 visualizações81 páginasfisiologi
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentofisiologi
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
100%(1)100% acharam este documento útil (1 voto)
142 visualizações81 páginasBody Fluids
Enviado por
clarintauchafisiologi
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 81
The Body Fluid Compartments
1. Extra cellular fluids (EFC)
a. Interstitial fluid
b. Plasma
c. Trans cellular fluid (1-2 liters)
- synovial fluid
- peritonel fluid
- pericardial fluid
- Intra ocular fluid
- Cerebrospinal fluid
2. Intra cellular fluid (ICF)
Body Fluid Compartment
TABEL 27.1 TOTAL BODY WATER AS A PERCENTAGE
OF BODY WEIGHT
Age Total body water, %
body weight
Newborn 77
6 months 72
2 years 60
16 years 60
20-39 years
Male 60
Female 50
40-59 years
Male 55
Female 47
Function of Waters
Water has many important and iterrelated
functions in the body. Some of the major ones are
the following :
1. It transports nutrients to cells and carries waste
products from cell
2. It provides a liquid medium for intracellular chemical
reactions, including overall cellular metabolism.
3. It acts as a solvent for electrolytes and other solutes.
4. It help maintain body temperature, aids digestion, and
pror excretion.
5. It transports enzymes, hormones, blood cells, and
many other substances.
Summary of body fluid regulation, including the major
body fluid compartments and the membranes that
separate these compartments. The values shown are for
an average 70-kilogram person.
* Fluid intake and output are balanced during
steady state conditions
Summary of sources of
water loss and gain per day
under normal conditions,
numbers are adult averages
Normal Prolonged
Heavy
Exercise
Intake
Fluids ingested 2100 ?
From metabolism 200 200
Total intake 2300 ?
Output
Insensible-Skin 350 350
Insensible-Lungs 350 650
Sweat 100 5000
Feces 100 100
Urine 1400 500
Total output 2300 6600
Daily Intake and Output of Water (in ml/day)
Fluid Exchanges. A diagrammatic representation of fluid movement
between the ICF and ECF, and between the ECF and the environment.
The volumes are not drawn to scale.
Blood Volume
- Blood contains : 1. Extra cellular fluid (the fluid
in plasma)
2. Intra cellular fluid (the fluid
in the red blood cells)
- The blood volume is especially important to the
control of cardiovascular dynamic
- The average blood volume of adults is about 7%
of body weight or about 5 liters
- 60% of the blood is plasma
- 40% of the blood is red blood cells
- These percentages depending on sex,
weight, and other factors
HEMATOCRIT (PACKED RED CELL VOLUME)
- The Hematocrit : is the fraction of the blood cells
as determined by centrifuging
blood in a hematocrit tube until
the cells become tightly packed
in the bottom of tube.
- 3 to 4 percent of the plasma remains eutrapped
among the cells.
- The true hematocrit is only about 96 percent of the
measured hematocrit.
- In men 0,40., Women 0,36.
- Anemia 0,10., Polycythemia 0,65.
CONSTITNENTS OF EXTRACELLULAR FLUID
- Ionic compositions of plasma and interstitial
Fluid are Similar.
- The plasma and interstitial fluid are separated
only by highly permeable capillary membranes.
- The plasma have high concentrations proteins.
- The capillaries have a low permeability to the
plasma protein.
- Creak only small amounts of protein into the
interstitial spaces in most tissues.
- Because of the Donan effect, the concentration
of cations (positively charged ions) is slightly
greater (about 2 percents) in the plasma than in
the interstitial fluids
- The plasma proteins have a net negative charge
tend to bind cations holding extra
amounts of these cations in the plasma along
with the plasma protein
- The interstitial fluid have higher concentration
anions than the plasma the negative
charges of the plasma proteins repel the
negatively charged anions
So : The concentration of ions in the interstitial
fluid and plasma are considered to be
about equal
Major cations and anions of the intracellular and
extracellular fluids
Nonelectrolytes of the plasma
Constituents of Intracellular Fluid
- The Intracellular fluid is separated from the
extracellular fluid by a selective cell membrane
- Selective cell membrane have highly permeable
to water, but not to most of the electrolytes in
the body
- It is contains :
* Small quantities of sodium ions
* Small quantities of chloride ions
* Almost no calcium ions
* Large amounts potassium ions
* Large amounts phosphate ions
* Moderate quantities of magensium and
sulfate ions
* Large amounts of protein, almost four
times as much as in the plasma
Measurement of Blood Fluid Volume
- Can use the indication principle
- Characteristic of the indicator dilution that used
to measure of the body fluid volume are :
1. The indicator disperses evenly
throughout the compartment
2. The indicator disperses only in the
compartment that is being measured
3. The indicator is not metabolized or
excreted
Indicator dilution method for measureing fluid volumes
Measurement of Body Fluid Volumes
Volume Indicators
Total body water 3H2O, 2H2O, antipyrine
Extracellular fluid 22Na, 125I-iothalamate, thiosulfate, inulin
Intracellular fluid (Calculated as Total body water
Extracellular fluid volume)
Plasma volume 125I-albumin, Evans blue dye (T-1824)
Blood volume 51Cr-Labeled red blood cells, or calculated
as Blood volume = Plasma volume/(1
hematrocit)
Interstitial fluid (Calculated as Extracellular fluid volume
2Plasma volume)
From Guyton AC, Hall JE: Human Physiology and mechanisms of
Disease. 6
th
ed. Philadelphia: WB Saunders Co, 1997.
Basic Concepts Pertaining to Fluid and
Electrolyte Regulations
- Four basic principles most be understood before
we can proceed to a discussion of fluid and
electrolyte balance.
- Concept 1 :All of the homeostatis mechanism
that monitor and adjust the composition of body
fluids respond to changes in the EFC, not in the
ICF
- Concept 2 : There are no receptors that can
directly monitor fluid and
electrolyte balance
- Concept 3 : Our cells are unable to move water
molecules by active transport
- Concept 4 : The body content of water or
electrolyte will rise if intake
exceeds outflow and fall if losses
exceed gains.
Movement of Body Water
-Movement of water from one body compartment
to another is controlled by two forces :
1. Hydrostatic pressure : is the force exerted by
a fluid against the surface of the
compartment containing the fluid
2. Osmotic pressure : is the pressure that most
be applied to a solution on one side of a
selectively permeable membrane to prevent
the osmotic flow of water across the
membrane from a compartment of pure water
- The cells membranes are highly permeable to
water but relatively impermeable even to small
ions such as sodium and chloride
- Water moves across the cell membrane
rapidly, so that the intracellular fluid remains
isotonic with the extracellular
- Osmosis : is the net diffusion of water across a
selectively permeable membrane from a region
of high water concentration to one that has a
lower water concentration
Relation Between Moles and Osmoles
- The water concentration of a solution depends
on the number of solute particles in the
solution a concentration term is needed to
describe the total concentration of solute
particles, regardless of their exact
composition
- Osmole : is the total nomber of particles in
solution
One (1) osmol = 1 mole (mol)(6.02 x 10
23
) of solution
particles
- 1 mol glucose/L has a concentration of 1 osm/L
- NaCl Na
+
+ Cl
-
(giving two ions)
1 mol NaCl/L will have an osmolar concentration
of 2 osm/L
The term osmole refers to the number of
osmotically active particles in a solution
rather than to the molar concentration
The osmole is too large a unit for expressing
osmotic activity of solutes in the body fluids
1 milliosmole = 1/1000 osmole
Osmolality and Osmolarity
- Osmolality : the osmolal concentration of
solution when it is expressed as osmoles per
kilogram of water
- Osmolarity : the osmolal concentration of
solution when its expressed as osmoles per
liter of solution
- These two terms can be used in dilute solution
(the body fluids) because the differences a small
- It is easier to express body fluid quantities in
liters of fluid rather than in kilograms of water in
most eases
- Most of the calculations used clinically and
clculations are based on osmolarities rather than
osmolalities
Relation Between Osmotic Pressure ad Osmolarity
-According to van's Hoffs law, osmotic pressure
() can be calculated ad
= CRT
: osmotic pressure mmHg
C : the concentration of solutes in osmoles per
liter
T : the absolute temperature indegree kelivin
(273o + centigrade) (273o + 37o = 310o kelvin)
R : The ideal gas constan
- The osmotic pressure of solution is directly
proportional to the concentration of
osmotically active particles in that solution.
- The solute used is not depend on large
molekul or small molekul
- Example : 1 mol albumin molecular
weight : 70.000
1 mol glucosa molecular
weight : 180
These have the same osmotic effect.
- One (1) molecular NaCl two (2) osmotically
active peticless Na
+
+ cl
-
has 2x the osmotic
effect
The osmotic pressure of a solution is
proportional to its osmolarity
- mmHg, T (273 + 37 = 310 Kelvin) The
value of Calculates to be about 19.300 mmHg
1 m0sm/L 19.3 mmHg.
For each milliosmole concentration gradient a
cross the cell membrane, 19.3 mmHg osmotic
pressure is eseerted
CALCULATION OF THE OSMOLARITY AND
OSMOTIC PRESSURE OF A SOLUTION
- Vans Hoffs law can use calculate the potential
osmotic pressure of a solution, assuming that
the cell membrane is impermeable to the solute
Example :
The osmotic pressure of 0,9% NaCl =
0,9% NaCl 0,9 gram/100 milliliter
MW NaCl : 58,5g/m molarity NaCl = 9 gram/L
: 58,5g/mol = 0,,154 mol/L
Each molecule of NaCl = 2 osmoles the
osmolarity of the solution is 0,154 x 2 = 308
osm/L
The potential osmotic pressure of this solution
= 308 mOsm/L x 19,3 mmHg/mOsm/L
= 5944 mmHg
There is correction factor called the osmotic
coefficient
Osmotic coefficient of NaCl is about 0,93
the actual osmolarity 0,9% NaCl = 308 x 0,93 =
286 mOsm/L
For practical reasons, sometimes the osmotic
coefficient of different solutes are neglected in
determining the osmolarity and osmotic
pressure of physiological solutions
Osmolarity of The Body Fluids
- 80% total osmolaroty of the intertitial fluid
and plasma is due to sodium and chloride ions
- Almost (50%) of the osmolality is due to
potassium ions in intracellular fluid
- Total osmolarity of each of the three compart
ments is about 300 m Osm/L, with the plasma
being about 1 m Osm/L greater that of the
intertitial and intracellular fluids caused by
the osmotic effects of the plasma poteins
maintain about 20 m Hg greater pressure in
capillaries than in the surrounding interstitial
space
- Total pressure averages about 5443 mmHg
for plasma; which is 19,3 times the correted
osmolarity of 282 m Osm/L for plasma
Osmotic Equilibrium is maintained between
intracellular and extracellular fluids
- Large osmotic pressure can develop a cross
the cell membrane with relatively small
changes in the concentration of solutes in
ECF
- As a result of these forces, relatively small
changes in concentration of impermeant
solutes in the ECF can cause tremen ions
changes in cell volume
- The efects of different concentration of
impermeant solutes in the extracellular fluid
on cell volume
* Isotonic : neither shrinks nor swells the cell
- If a cell is placed in a solution of
impermeant solutes having an osmolarity
of 282 mOsm/L, the cells will not shrink or
swell because the water concentrations in
the intracellular and extracellular fluids are
equal and the solutes cannot enter or leave
the cell
- Examples of isotonic solutions are :
* 0,9 percent NaCl solution
* 5 percent glucose solution
- These solution are important in clinical
medicine because they can be infused into
the blood without the danger of upsetting
osmotic equilibrium between the
intracellular and extracellular fluid
* Hypo tonic : there is cell swells
- If a cells is placed in a solution of
impermeant solutes having a osmolarity of
200 m Osmol/L (lower concentration or
less than 282 m Osm/L, water will diffuse
into the cell, causing it to swell
- Water will continue to diffuse into the cell,
diluting the intracellular fluid until both
solution have about the same osmolarity
- Example : solutions of NaCl with a
concentration of less than 0,9 percent
* Hyper tonic : there is cell shrinks
- If a cell is placed in a hyper tonic solution
have a lughed concentration of
impermeant solutes, water will flow out of
the cell into the ECF, concentrating the ICF
and diluting the ECF
- In this case, the cell will shrink until the two
concentration become equal
- Example : solutions of NaCl with
concentration of greater than 0,9 percent
Figure : Effects of isotonic (A) hyper tonic (B), and hypo
tonic (C) solutions on cell volume
- The terms isomotic, hyper osmotic and
hypo osmotic are used to describe the changes
in volume (i.e. dehydration and overhydration)
and refer to the ECF in its new steady state
* Isomotic : the term of the solutions
regardless of iohether the solute can
penetrate the cell membrane or not
* Hypo osmotic : the term of the solutions
with a lower osmolarity compared with
normal ECF, without regard for whether the
solute permeates the cell membrane
* Hyper osmotic : the term of the solution
have a higher osmolarity than the normal
ECF, without regard for whether the solute
permeates the cell membrane
- Osmotic equilibrium between ICF and ECF is rapidly
attained
- This rapid movement of water across the cell membrane
does not mean that complete equilibrium occurs between
the intracellular and extracellular compartments
throughout the whole body within the same short period
that fluid usually enters the body through the gut and
must be transported by the blood to all tissue before
complete osmotic equilibrium can occur
- It usually takes about 30 minutes to achieve osmotic
equilibrium every where in the body after drinking water
Volume and Osmolalities of ECF an ICF in
Abnormal State
- Some of the different factors that can cause
ECF and ICF volumes to change markedly are
- Ingestion of water
- Debydration
- Loss of large amounts of fluid from the GIF
- Loss sweating or through the kidney
Basic principles that have to kept in mind :
1. Water moves rapidly across cell membranes;
therefore, the osmolarities of ICF and ECF
remain almost exactly equal to each other
except for a few minutes after a change in one
of the compartments
2. Cell membranrs are almost completely in
permeable to many solutes; therefore, the
number of osmoles in ECF and ICF remains
constant unless solutes are added to or lost
from the extracellular compartment
We can analize the effects of different
abnormal fluid conditions on ECF + ICF
volumes and osmolarities
* Effect of Adding Saline Solution to The ECF
Effect of adding isotonic, hypertonic, and hypotonic solutions to the
extracellular fluid after osmotic equilibrium. The normal state is indicated by
the solid lines, and the shifts from normal are shown by the shaded areas.
The volumes of intracellular and extracellular fluid compartment are shown in
the abscisa of each diagram, and the osmolarities of these compartment are
shown on the ordinates.
The general clinical terms for volume
abnormalities are :
1. Dehydration
2. Overhydration
A. Dehydration (Volume Contraction) State
a. Isosmotic Dehydration (see fig. 4-2 A1)
(1) Description
- Initially, fluid is lost from the plasma and then is
repleted from the interstitial space. No major
change occurs in the osmolality of the ECF;
therefore, no fluid shifts into or out of the ICF
compartment
- Finally, the volume of the ECF is reduced with no
change in osmolality
(2) Causes of isosmotic dehydration include
hemorrhage, plasma exudation through burned
skin, and gastrointestinal fluid loss (e.g. vomiting
and diarrhea)
b. Hyperosmotic Dehydration (see Fig. 4-2 A2)
(1) Description
a. Initially, fluid is slot from the plasma, which
becomes hyper osmotic, causing a fluid shift
from the interstitial fluid to the plasma
b. The rise in interstitial fluid osmolality causes
fluid to shift from the ICF to the ECF
compartment
c. Finally, the ECH and ICF volumes both are
decreased, and the osmolality of both major
fluid compartments is increased
(2) Cause of hyperosmotic dehydration include
water deficits due to decreased intake, diabetes
insipidus (neurogenic or nephrogenic),
alcoholism, administration of lithium salts,
fever, and excessive evaporation from the skin
and breath
c. Hyposmotic Dehydration (see Fig. 4-2 A3)
(1) Description
a. Initially, loss of sodium chloride (NaCl)
causes a loss of water. This is followed by
water retention but a continued loss of NaCl.
b. A net loss of NaCl in excess of water loss
results in a decreased osmolality of the ECF
and a subsequent shift of fluid from the ECF
to the ICF compartment
c. Finally, the ECF volume is decreased, the ICF
volume is increased, and the osmolality of
both major fluid compartments is decreased
(2) Causes of hyposmotic dehydration include
loss of NaCl due to heavy loss of hypo tonic
sweat and renal loss of NaCl due to adrenal
insufficiency (e.g. primary
hypoadrenocorticalism or Addisons disese)
B. Over hydration (Volume Expansion) State
a. Isosmotic Over hydration (see Fig. 4-2 B1)
(1) Description. Isosmotic over hydration is
characterized by an overall expansion of the
ECF volume with no change in the
osmolality of the ICF and ECF compartments.
(2) Causes of isosmotic over hydration are edema
and oral or parental administration of a large
volume of isotonic NaCl
b. Hyperosmotic Overhydration (see Fig. 4-2 B2)
(1) Description
a. Initially, there is water retention followed by
NaCl retention in excess of water
b. The rise in plasma osmolality causes a
shift of water from the ICF to the ECF
compartment
c. Finally, the ECF volumes is expanded, the
ICF volume is contracted, and the osmolality
of both major fluid compartments is increased
(2) Cause. Oral or parental intake of large amounts
of hyper tonic fluid causes hyperosmotic
overhydration
c. Hyposmotic Overhydration (see fig. 4-2 B3)
(1) Description
a. Initially, water enters the plasma, causing a
decline in the plasma osmolality, a shift of
water into the interstitial space, and a
decrease in the interstitial fluid osmolality
b. The decrease in interstitial fluid osmolality
causes water to shift from the ECF to the ICF
compartment
c. Finally, the ECF and ICF volumes increase
and the osmolality of both major fluid
compartments decreases
(2) Causes of hyposmotic overhydration include
ingestion of a largevolume of water and renal
retention of water due to the syndrome of
inappropriate antidiuretic hormone (ADH)
secretion (SIADH)
Steady State Change in Volume and Osmolal Concentration of Body Fluids
Volume (L) Osmolality(mOsm/kgH2O)
Type of Change ICF ECF ICF ECF
Contraction (dehydration)
Isosmotic 0 0
Hyperosmotic
Hyposmotic
Expansion (overhydration)
Isosmotic 0 0 0
Hyperosmotic
Hyposmotic
Note. The changes in volume and in osmolality refer to the ECF
compartment in the new steady state
There is a good correlation between the ICF volume and total exchangeable
K+. ICF volume also is related to muscle mass, which decreases with age.
Glucose and other solutions administered for
nutritive purposes
- Many types of solution are administered in
travenously :
* Glucose solution widely used
* Amino acid and homogenized fat solution are
used to lesser extent
- When there solutions are administered;
* Their concentrations of osmotically active substances
are usually adjusted nearly to isotonicity
* They are given slowly enough that they dont up set the
osmotic equilibria of the body fluids
- After the glucose or other nutrients are
metabolized an excess of water often
remains, especially if additional fluid is
ingested
So. The net result is addition only of the
nutrients to the body and the dilute urine
was excreted from the kidneys
EDEMA : Excess fluid in the tissue
- The presence of excess fluid in the body
tissue
- EDEMA : 1. Intracellular Edema
2. Extarcellular Edema
1. Intracellular Edema
Cause : a. depression of the metabolic system
of the tissue
b. lack of adequate nutrition to the
cells
Example :
Blood flow the delivery of oxygen and
nutrients the cell membrane ionic pumps
(depressed) sodium cannot be pumped
out of the cells and the excess sodium ions
inside the cells cause osmosis of water into
the cells volume intracellular of a tissue
area even of an entire is chemic leg
prelude to death of the tissue
The inflamed tissue the cell membranes
permeability sodium + other ions into the
interior of the cell
2. Extracellular Edema
- Excess fluid accumulation in the
extracellular space
- Cause :
a. Abnormal leakage of fluid from the
plasma to the interstitial spaces across
the capillaries
b. Failure of the lymphation to return fluid
from the interstitium back into the blood
c. Increase capillary fluid filtration
Filtration = Kf x (Pc Pif - c + if)
Kf : the capillary filtration coefficient
Pc : the capillary hydrostatic pressure
Pif : the interstitial
c : the capillary plasma colloid osmotic
pressure
if : the interstitial fluid colloid osmotic
pressure
Different conditions that can cause
extracellular edema
I. Increased capillary pressure
A. Excessive kidney retention of salt and
water
1. Acute or chronic kidney failure
2. Mineralocorticoid excess
B. High venous pressure
1. Heart failure
2. Venous obstruction
3. Failure of venous pumps
(a) Paralysis of muscle
(b) immobilized parts of body
(c) failure of venous valves
C. Decreased arteriolar resistance
1. Excessive body heat
2. Insufficiency of sympathetic nervous system
3. Vasodilator drugs
II. Decreased plasma proteins
A. Loss of proteins in urine (nephrotic syndrome)
B. Loss of protein from denuded skin areas
1. Burns
2. Wounds
C. Failure to produce proteins
1. Liver disease
2. Serious protein or caloric malnutrition
III. Increased capillary permeability
A. Immune reactions that cause release of histamine
and other immune products
B. Toxins
C. Bacterial infections
D. Vitamin deficiency, especially vitamin C
E. Prolonged eschemia
F. Burns
IV. Blockage of lymph return
A. Cancer
B. Infections (e.g., filaria nematodes)
C. Surgery
D. Congenital absence or abnormality of lymphatic
vesels
Safety factors that normally prevent edema
- Even through many disterbances can cause
edema, usually the abnormality must be severe
before serious edema develops
- There are three major safety factors prevent
fluid accumulation in the interstitial space :
1. How compliance of the interstitium when
interstitial fluid pressure is in the negative
pressure range (is about 3 mm Hg)
2. The ability of lymph flow to increase 10 to 50 fold
(is about 7 mm Hg)
3. Wash down of interstitial fluid protein
concentration, which reduces interstitial fluid
colloid osmotic pressure as (is about 7 mm Hg)
The total safety factor against edema is
about 17 m Hg the capillary pressure in
periperal tissue could theoretically rise by
17 mm Hg or approximately double the
normal value, be fore edema would accur
Fluids in the Potential spaces of the
body
-Many types of potential space
Example : * The pleural cavity
* The pericardial cavity
* The peritoneal cavity
* The synovial cavities
* The joint cavities
* The joint bursae
- All there potential space have surfaces that
almost touch each other with only a thin layer of
fluid in between, the surface slide over each
other
- To facilitate the sliding a viscous protemaceous
fluid lubricates the surfaces
- Fluid is exchanged between the capillaries and
the potential space
- Lymphatic vessels drain protein from the
potential spaces
- Edema fluid in the potential sapces is called
effusion
Example : - gelular effesion
- ascites abdominal
cavity
- In serious cases, 20 liters or more ascitic fluid
can accumulate
- The pleural cavity, pericardial cavity, and joint
spaces can become seriously swollen when
there is generalized edema
- Injury or local infection in any one of the cavities
often blocks the lymph drainage, causing
isolated swelling in any one of the cavities
- Normal fluid pressure in most or all of the
potential spaces in the nonedema tour state
is negative in the same way that this pressure
is negative in lease subcutaneous tissue
- Interstitial fluid hydrostatic pressure is
normaly about 7 to 8 mm Hg in the pleural
cavity, -3 to 5 mm Hg in the joint soace, and
-5 to 6 mm Hg in the pericardial cavity
Você também pode gostar
- Body Fluids Hbc202-Lecture Notes-1Documento9 páginasBody Fluids Hbc202-Lecture Notes-1Shreya AnandAinda não há avaliações
- Body FluidsDocumento44 páginasBody FluidsO'Brien Alfred100% (1)
- Blood Vessels and Lymphatics in Organ SystemsNo EverandBlood Vessels and Lymphatics in Organ SystemsDavid AbramsonAinda não há avaliações
- BloodDocumento38 páginasBloodchukwukerechimezirimAinda não há avaliações
- Sweet Biochemistry: Remembering Structures, Cycles, and Pathways by MnemonicsNo EverandSweet Biochemistry: Remembering Structures, Cycles, and Pathways by MnemonicsAinda não há avaliações
- Body Fluids and ElectrolytesDocumento42 páginasBody Fluids and ElectrolytesQusaiBadr100% (1)
- Water LoseDocumento29 páginasWater LoseJAKLIN EMPOLAinda não há avaliações
- Composition and Function of Blood ComponentsDocumento17 páginasComposition and Function of Blood ComponentsPrakash Kumar Nayak100% (1)
- Anatomy and Physiology Summary Body Fluids and BloodDocumento22 páginasAnatomy and Physiology Summary Body Fluids and BloodKelly Anne BrandAinda não há avaliações
- MCQ MembranesDocumento10 páginasMCQ MembranesMarilyne RizkAinda não há avaliações
- The Fate of Metabolism Andmabolic PathwaysDocumento25 páginasThe Fate of Metabolism Andmabolic PathwaysXuân Vi100% (1)
- The Physiology of BloodDocumento41 páginasThe Physiology of BloodDr.M.Anthony David100% (10)
- Physiology, Lecture 4, Blood (Slides)Documento28 páginasPhysiology, Lecture 4, Blood (Slides)Ali Al-QudsiAinda não há avaliações
- Blood PhysiologyDocumento82 páginasBlood PhysiologyVioleta Voinovan100% (2)
- Body Fluids and Fluid CompartmentsDocumento7 páginasBody Fluids and Fluid CompartmentsAditya Shrivastava100% (1)
- Reverse Cholesterol TransportDocumento29 páginasReverse Cholesterol TransportSolomon RotimiAinda não há avaliações
- Lecture 2 - HomeostasisDocumento27 páginasLecture 2 - HomeostasisAndre Luis CostaAinda não há avaliações
- Chapter 70-GuytonDocumento9 páginasChapter 70-Guytonswoljaswol1Ainda não há avaliações
- Fluids and Electrolytes-2Documento82 páginasFluids and Electrolytes-2Jem Loterte100% (1)
- Physiology QuestionsDocumento14 páginasPhysiology QuestionsLamis Alhaj KaddamAinda não há avaliações
- Physiology Comprehensive Exam Pointers PDFDocumento108 páginasPhysiology Comprehensive Exam Pointers PDFRaynalynGimoros100% (1)
- Acidification of UrineDocumento30 páginasAcidification of UrineNanditha SureshAinda não há avaliações
- DLC PracticalDocumento6 páginasDLC PracticalAngoruz Gohain BaruahAinda não há avaliações
- BloodDocumento103 páginasBloodrizwanbas50% (2)
- Urinary SystemDocumento2 páginasUrinary SystemCharlayne AnneAinda não há avaliações
- Endocrine System Review Flashcards - QuizletDocumento5 páginasEndocrine System Review Flashcards - QuizletDani Anyika100% (1)
- Blood 12-6-2018Documento42 páginasBlood 12-6-2018Noor Fatima100% (1)
- Renal PhysiologyDocumento193 páginasRenal Physiologyramadan100% (1)
- Disorders of Calcium and Phosphate MetabolismDocumento20 páginasDisorders of Calcium and Phosphate MetabolismThirupathi Jakkani100% (1)
- Tutorial Lymphatic SystemDocumento3 páginasTutorial Lymphatic SystemHazwan100% (1)
- Chapter 20 QuestionsDocumento10 páginasChapter 20 QuestionshenrikayeAinda não há avaliações
- BloodDocumento197 páginasBloodNimesh Sharma100% (1)
- Skeletal Muscle Contraction QuestionsDocumento2 páginasSkeletal Muscle Contraction Questionsgoofy_jess25% (4)
- Urine Formation: Reabsorption and Secretion, and Water ConservationDocumento5 páginasUrine Formation: Reabsorption and Secretion, and Water ConservationAshraf Moby100% (1)
- Acidification of UrineDocumento19 páginasAcidification of UrineRakeshkumar Pradhan100% (1)
- Gastrointestinal PhysiologyDocumento134 páginasGastrointestinal Physiologyapi-19916399100% (1)
- 1 Body FluidsDocumento9 páginas1 Body FluidsSenthereng MoaisiAinda não há avaliações
- Presented By: DR Sharmila G SDocumento76 páginasPresented By: DR Sharmila G SSharmila Shivakumar G SAinda não há avaliações
- The Body As A Whole: Introduction To The Human BodyDocumento90 páginasThe Body As A Whole: Introduction To The Human BodyLudy Mae NalzaroAinda não há avaliações
- Renal PhysiologyDocumento75 páginasRenal PhysiologyAmanuel Maru100% (1)
- Acid Base BalanceDocumento35 páginasAcid Base BalanceDhanasvi Dessai100% (1)
- Unit 3: Control and Regulation: Physiological HomeostasisDocumento16 páginasUnit 3: Control and Regulation: Physiological HomeostasisaclumutAinda não há avaliações
- Fluid and Electrolyte Imbalance and Nutritional ProblemDocumento98 páginasFluid and Electrolyte Imbalance and Nutritional ProblemPaul EbenezerAinda não há avaliações
- Red Blood Cell CountDocumento4 páginasRed Blood Cell CountMohamed MokhtarAinda não há avaliações
- MCQs in Fluid and Electrolyte Balance With AnswersDocumento50 páginasMCQs in Fluid and Electrolyte Balance With AnswersAbdulkadir Waliyy Musa100% (2)
- Physiology of Body FluidsDocumento23 páginasPhysiology of Body FluidsRamadan Physiology100% (1)
- Histology, Lecture 6, Connective Tissues (Lecture Notes)Documento6 páginasHistology, Lecture 6, Connective Tissues (Lecture Notes)Ali Al-Qudsi100% (3)
- Body Fluids Fluid Physiology NotesDocumento19 páginasBody Fluids Fluid Physiology NotesBrianAinda não há avaliações
- MCQs & QUs On Fsirst Year First ComDocumento74 páginasMCQs & QUs On Fsirst Year First Commaisara10Ainda não há avaliações
- Titrable Acidity of UrineDocumento2 páginasTitrable Acidity of Urinewardahkhattak100% (2)
- Topic - Composition of BloodDocumento18 páginasTopic - Composition of BloodChhavi SainiAinda não há avaliações
- 2012-Fluid and ElectrolytesDocumento192 páginas2012-Fluid and ElectrolytesHarley Justiniani Dela CruzAinda não há avaliações
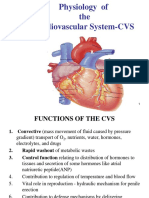
- Physiology of The Cardiovascular System-CVSDocumento56 páginasPhysiology of The Cardiovascular System-CVSAmanuel MaruAinda não há avaliações
- CARDIAC CYCLE - Part I PDFDocumento55 páginasCARDIAC CYCLE - Part I PDFChirag Dagar100% (1)
- Blood Cells and Its Types With FunctionsDocumento5 páginasBlood Cells and Its Types With Functionskaleb16_2Ainda não há avaliações
- Kreb CycleDocumento6 páginasKreb Cycle211BT014 Jeev Sheen JosephAinda não há avaliações
- Introduction To Cell PhysiologyDocumento39 páginasIntroduction To Cell Physiologywaqas_xsAinda não há avaliações
- Lecture On Resting Membrane Potential by DR RoomiDocumento18 páginasLecture On Resting Membrane Potential by DR RoomiMudassar Roomi67% (3)
- GIT EmbryologyDocumento162 páginasGIT EmbryologywahyuAinda não há avaliações
- Presentation Title: Subtitle Goes HereDocumento2 páginasPresentation Title: Subtitle Goes HereclarintauchaAinda não há avaliações
- Becoming By: JournalDocumento1 páginaBecoming By: JournalclarintauchaAinda não há avaliações
- Myoma 1Documento3 páginasMyoma 1clarintauchaAinda não há avaliações
- Am J Clin Nutr 2000 Sermet Gaudelus 64 70Documento7 páginasAm J Clin Nutr 2000 Sermet Gaudelus 64 70clarintauchaAinda não há avaliações
- 4 Miller Ncac-Sot 5'08Documento42 páginas4 Miller Ncac-Sot 5'08clarintauchaAinda não há avaliações
- The Effect of Severe Early Malnutrition On Cellular Growth Human BrainDocumento4 páginasThe Effect of Severe Early Malnutrition On Cellular Growth Human BrainclarintauchaAinda não há avaliações
- Follow Up: S O A P Keluhan Status Assesment PenatalaksanaanDocumento1 páginaFollow Up: S O A P Keluhan Status Assesment PenatalaksanaanclarintauchaAinda não há avaliações
- Tugas Ebm: Judul JurnalDocumento2 páginasTugas Ebm: Judul JurnalclarintauchaAinda não há avaliações
- 1901 - Lewis - The Law of Physico-Chemical ChangeDocumento21 páginas1901 - Lewis - The Law of Physico-Chemical ChangemontoyazumaetaAinda não há avaliações
- Chapter14 (Solutions)Documento96 páginasChapter14 (Solutions)Kaye DomingoAinda não há avaliações
- Dehradun Region, Class Xii, Chemistry, Study MaterialDocumento177 páginasDehradun Region, Class Xii, Chemistry, Study MaterialgudiAinda não há avaliações
- osmosis colligative: α Swante Arrenius, Wilhelms Ostwalds 1886.gadā Rīgā αDocumento12 páginasosmosis colligative: α Swante Arrenius, Wilhelms Ostwalds 1886.gadā Rīgā αJane IvanovaAinda não há avaliações
- Pore PressureDocumento15 páginasPore PressureVinod ParamataAinda não há avaliações
- Test Bank For Chemistry General Organic and Biological 10th Edition Karen Timberlake Download Full DownloadDocumento18 páginasTest Bank For Chemistry General Organic and Biological 10th Edition Karen Timberlake Download Full Downloadsaraboydtfwqybmone100% (40)
- CALCULATIONS INVOLVING SOLUTIONS - Student'sDocumento5 páginasCALCULATIONS INVOLVING SOLUTIONS - Student'sMarco Bose100% (1)
- SOLUTIONS Formula Sheet PDFDocumento4 páginasSOLUTIONS Formula Sheet PDFVansh YadavAinda não há avaliações
- Minimum Learning Material XiiDocumento27 páginasMinimum Learning Material XiiSmv KumAinda não há avaliações
- 8 Chapter 12 1Documento51 páginas8 Chapter 12 1azizAinda não há avaliações
- SolutionsDocumento32 páginasSolutionsMayuresh PanseAinda não há avaliações
- Chapter 16 SolutionsDocumento92 páginasChapter 16 SolutionsPeter PanAinda não há avaliações
- Continuing The Journey Amongst Mangroves - Clough - 2013 Part IDocumento100 páginasContinuing The Journey Amongst Mangroves - Clough - 2013 Part IhanggarPKAinda não há avaliações
- Polymer Science: Molecular Weights of PolymersDocumento22 páginasPolymer Science: Molecular Weights of PolymersMeeit GuleriaAinda não há avaliações
- Questions: of Asked in Previous BoardDocumento24 páginasQuestions: of Asked in Previous BoardNeet NightsAinda não há avaliações
- Physical Properties of SolutionsDocumento67 páginasPhysical Properties of SolutionsFABIO DE LIMAAinda não há avaliações
- Polymer PhysicsDocumento405 páginasPolymer PhysicsPurushothaman100% (6)
- Diffusion and OsmosisDocumento6 páginasDiffusion and OsmosisWacoomo TaroomaAinda não há avaliações
- How Is Henry's Law Constant K 8. How Is Solubility of A Gas in A Liquid Related To Temperature?Documento6 páginasHow Is Henry's Law Constant K 8. How Is Solubility of A Gas in A Liquid Related To Temperature?Snehashis BoseAinda não há avaliações
- Water Treatment - Reverse OsmosisDocumento217 páginasWater Treatment - Reverse OsmosisDangolAinda não há avaliações
- 2.solutions FDocumento33 páginas2.solutions Fshrutianand8915Ainda não há avaliações
- Biochemistry Lab Hand OutsDocumento12 páginasBiochemistry Lab Hand Outsrica sebabillonesAinda não há avaliações
- ACT Crack ChemistryDocumento157 páginasACT Crack ChemistryabdogamreAinda não há avaliações
- 2 HoursDocumento17 páginas2 HoursOTTO OLIMAAinda não há avaliações
- 02 The Chemistry of Milk PDFDocumento26 páginas02 The Chemistry of Milk PDFTintin Brusola SalenAinda não há avaliações
- Report 115Documento44 páginasReport 115Mouhamed NdongAinda não há avaliações
- General Chemistry 2: Quarter 3 - Week 4Documento20 páginasGeneral Chemistry 2: Quarter 3 - Week 4Anime KISSANIME100% (1)
- Reverse OsmosisDocumento19 páginasReverse Osmosiswaqasali12250% (2)
- Pharmaceutical CalculationsDocumento37 páginasPharmaceutical Calculationsanon_93799477850% (2)
- Transport in PlantsDocumento7 páginasTransport in PlantsRiya SharanAinda não há avaliações