Escolar Documentos
Profissional Documentos
Cultura Documentos
Good Morning Report!: Nora Switchenko MD R3
Enviado por
Emily EresumaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Good Morning Report!: Nora Switchenko MD R3
Enviado por
Emily EresumaDireitos autorais:
Formatos disponíveis
Good morning report!
Nora Switchenko MD R3
The Case
ID: 10 year old female presents to the emergency room
CC: Joint pain
HPI:
Subjective fevers on and off for about 2 weeks
Right ankle pain started about 10 days ago. There was ankle
swelling but no erythema. Pain was about 5/10. Constant. Ankle
swelling and pain has improved and barely present at time of
presentation.
Left knee pain started yesterday. +swelling but no erythema.
Pain is severe 8/10 and causes limp.
Joint pain improves with NSAID, but patient still does not want to
walk
Other symptoms: mild nausea
Negatives: no V/D, no URI/cold symptoms now or in the past few
weeks, no sore throat, no rash, no abnormal limb movements, no
SOB
Prior to presentation in the emergency room, patient had normal
xrays of right ankle and negative rapid strep testing.
The Case
PMedHx: Healthy
FamilyHx: No acute illnesses, no autoimmune diseases
SocialHx: Home with siblings for summer vacation. No
known sick contacts.
The Case
VITALS: TEMP 38.7, HR 105, RR 23, BP 102/50
PHYSICAL EXAM:
GENERAL: Comfortable, lying on exam table
HEENT: NC/AT, conjunctiva clear, no nasal drainage, OP with mild
erythema without exudate, no palatal petechiae, TMs gray with positive
light reflex bilaterally
RESP: CTAB, no increased WOB, no crackles, excellent air movement
CV: RRR, normal S1 and S2, pansystolic 2/6 murmur heard best at LLSB,
distal pulses 2+ in UEs and LEs
ABDO: Soft, NTND, no HSM, BS+
MSK: Right ankle has mild swelling without erythema or warmth and no
pain with palpation, Left knee has moderate swelling without erythema
and is warm to the touch. There is some pain with motion but patient has
FROM in right knee as well as all other joints. Able to stand but walks with
significant limp.
NEURO: CN 2-12 intact, 5/5 strength in UEs and LEs, normal tone, gait is
limited by limp on right knee
SKIN: No rash on face, extremities, abdomen, chest or back.
Differential diagnosis
10 year old female with fever, murmur, and polyarthritis.
Differential diagnosis
10 year old female with fever, murmur, and polyarthritis.
ID
Septic arthritis
Osteomyelitis
Endocarditis
Other bacterial infections
(TB, Gonococcus, Brucella,
Lyme)
Viral Infections (Hep B and
C, Rubella, Parvovirus)
Heme/Onc
Hemarthrosis
ALL
Neuroblastoma
Sickle cell anemia
Rheum
Post infectious reactive arthritis
Juvenile idiopathic arthritis
Rheumatic fever
Lupus
Familial Mediterranean fever
Juvenile dermatomyositis
Sarcoidosis
Henoch-Schonlein purpura
Ankylosing spondylitis
Psoriatic arthritis
Rheumatoid arthritis
Serum sickness
IBD associated arthritis
The Case
ED work up:
WBC 9.9, Hgb 9.9 (MCV80), Plts 483
CRP 18.9
ESR 131
ASO 545 H
AntiDNAaseB 478 H
Rapid strep positive
EKG showed normal sinus rhythm without PR prolongation
Diagnosis: Rheumatic Fever
Treatment: Amoxicillin for step throat, ibuprofen for joint
pain
Disposition: Cardiology clinic visit and ECHO scheduled for the
following morning
The Case
ECHO results:
Mild aortic valve regurgitation
Mild mitral valve regurgitation
Normal left and right ventricular size and qualitatively normal
systolic function
Plan of care:
Continue amoxicillin
High dose aspirin (80-100 mg/kg) until acute phase reactants
normalize
Following amoxicillin, start penicillin G IM q 4 weeks
Rest until carditis resolves
Follow up in one week for repeat labs, aspirin level (goal <30 mg/dl)
Rheumatic Fever : Diagnosis
Diagnosis is made clinically with evidence of preceding GAS infection and either 2
major or 1 major and 2 minor Jones criteria.
Jones Criteria
Evidence of preceding GAS infection
Positive throat culture
Positive rapid streptococcal antigen test
Elevated or rising streptococcal antibody titer (ASO, antiDNAase B)
Major
Migratory arthritis
Carditis
CNS effects (Sydenham chorea)
Erythema marginatum
Subcutaneous nodules
Minor
Arthralgia
Fever
Elevated inflammatory markers
Prolonged PR interval
Major Criteria: Migratory arthritis
Typically the first symptom present
Involves several joints in quick succession
Larger joints more commonly involved
LE usually involved first
May be severe enough to limit movement or
cause a limp
Synovial fluid demonstrates sterile
inflammation
NSAIDs may alter natural course of disease
Major Criteria: Carditis
Pancarditis including valvulitis
Mitral valve involved in nearly all cases
Aortic valve involved in 20-30% of cases
Severe carditis can lead to dilated
cardiomyopathy and heart failure
Conduction abnormalities possible
Recurrent episodes of rheumatic fever lead
to cumulative damage to heart and possible
to rheumatic heart disease
Major Criteria: CNS effects
Sydenhams chorea: abrupt,
nonrhythmic, involuntary
movements
Muscular weakness
Emotional lability
Can be a delayed manifestation of
RF
Improves gradually over 12-15
weeks
Full recovery seen in almost all
patients
Risk of recurrence 20-30% with
subsequent GAS infection
Major Criteria: Erythema marginatum and
Subcutaneous nodules
Rheumatic Heart Disease: Treatment
Primary prevention treat GAS pharyngitis
3 goals of treatment
Symptomatic relief
Aspirin 80-100 mg/kg/day
Eradication of GAS
Amoxicillin 50 mg/kg/day divided BID for 10 days
Prevention of future GAS infection to avoid further
cardiac damage (Secondary prevention
Penicillin injections until adulthood
Rheumatic heart disease
Valve replacement or repair
Congestive heart failure management
References
1. John, J. Arthritis in Children and Adolescents. Pediatrics
in Review Vol. 32 No. 11 November 1, 2011
2. WHO Expert Consultation on Rheumatic Fever and
Rheumatic Heart Disease 2001
3. Burke, RJ. Diagnostic criteria of acute rheumatic fever.
Autoimmun Rev. 2014 Apr-May;13(4-5):503-7
Pediatrics in Review
Você também pode gostar
- Lupus Case PresentationDocumento48 páginasLupus Case PresentationRoscelie KhoAinda não há avaliações
- IVIgDocumento2 páginasIVIgernestjohnAinda não há avaliações
- Pyloric StenosisDocumento16 páginasPyloric StenosisHelen McClintockAinda não há avaliações
- Pediatrics: 2 Case ReportDocumento50 páginasPediatrics: 2 Case ReportSam Raven AndresAinda não há avaliações
- IM AdconDocumento28 páginasIM AdconCla SantosAinda não há avaliações
- Cataract: Case Presentation - M.E.T.H.O.DDocumento7 páginasCataract: Case Presentation - M.E.T.H.O.DKismet SummonsAinda não há avaliações
- Pedia - DengueDocumento10 páginasPedia - DengueJan Mikhail FrascoAinda não há avaliações
- Assessment Diagnosis Planning Interventions Rationale Evaluation Subjective: IndependentDocumento3 páginasAssessment Diagnosis Planning Interventions Rationale Evaluation Subjective: IndependentAce Khiel PeraltaAinda não há avaliações
- Simple Purpura (Easy Bruising Syndrome)Documento4 páginasSimple Purpura (Easy Bruising Syndrome)Rebecca WongAinda não há avaliações
- Case AppendicitisDocumento30 páginasCase AppendicitisSarahAinda não há avaliações
- Polycythemia in NewbornDocumento25 páginasPolycythemia in NewbornTheva Thy100% (2)
- Background: Viral Mumps InfectionDocumento5 páginasBackground: Viral Mumps InfectionAgustin UyAinda não há avaliações
- Hiv Case StudyDocumento2 páginasHiv Case Studyapi-485814878Ainda não há avaliações
- Pyloric StenosisDocumento11 páginasPyloric StenosisJustin CharlesAinda não há avaliações
- LA Myxoma Case PresentationDocumento34 páginasLA Myxoma Case PresentationWiwik Puji LestariAinda não há avaliações
- Pediatrics 2 LaboratoryDocumento40 páginasPediatrics 2 LaboratoryAmaetenAinda não há avaliações
- Glomerulonephritis PresentationDocumento23 páginasGlomerulonephritis Presentationjacksonyu1234Ainda não há avaliações
- Management of Tuberculosis: A guide for clinicians (eBook edition)No EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Ainda não há avaliações
- HERNIA - Case StudyDocumento8 páginasHERNIA - Case StudyMa Jaimeliz Mae MuñizAinda não há avaliações
- Inguinal Hernia MinicaseDocumento13 páginasInguinal Hernia MinicaseGerold Chua100% (1)
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- Cerebrovascular Disease (Bleed)Documento25 páginasCerebrovascular Disease (Bleed)Margaret Jenaw JenawAinda não há avaliações
- Post-Streptococcal GlomerulonephritisDocumento18 páginasPost-Streptococcal GlomerulonephritisPreciousJemAinda não há avaliações
- Cough and Dyspnea Case StudyDocumento4 páginasCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Tuberculosis and Nephrotic Syndrome in A Child: Case ReportDocumento34 páginasTuberculosis and Nephrotic Syndrome in A Child: Case ReportAldo YustiantoAinda não há avaliações
- Opd CaseDocumento13 páginasOpd CaseRaven CièlAinda não há avaliações
- Diarrhea 2016Documento37 páginasDiarrhea 2016oli garkiAinda não há avaliações
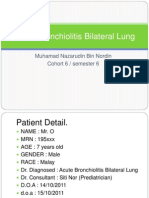
- Acute Bronchiolitis Bilateral Lung Case Study PresentationDocumento36 páginasAcute Bronchiolitis Bilateral Lung Case Study PresentationPyka Izzaty100% (1)
- Acute Hypertension-Hypertensive Urgency and Hypertensive EmergencyDocumento13 páginasAcute Hypertension-Hypertensive Urgency and Hypertensive EmergencyAmitKumarAinda não há avaliações
- Case Presentation - GBSDocumento28 páginasCase Presentation - GBSJan Marvin Lichauco MendozaAinda não há avaliações
- Progress NoteDocumento3 páginasProgress NoteHaji JawaroAinda não há avaliações
- Case 6: Delos Reyes, Lasac, Majid, Mamangun, YuDocumento49 páginasCase 6: Delos Reyes, Lasac, Majid, Mamangun, YuAbdullah Bin MajidAinda não há avaliações
- Course in The WardDocumento3 páginasCourse in The WardAljon S. TemploAinda não há avaliações
- Case Report Pediatric Von&JepDocumento23 páginasCase Report Pediatric Von&JepFarizan NurmushoffaAinda não há avaliações
- GE BasavaDocumento21 páginasGE BasavaAmalin PrãdhãñAinda não há avaliações
- DOH ProgramsDocumento6 páginasDOH ProgramsMichael VillavertAinda não há avaliações
- Case Presentation: by Michael ArmstrongDocumento21 páginasCase Presentation: by Michael ArmstrongWirawan Amirul BahriAinda não há avaliações
- RabiesDocumento10 páginasRabiesWinda LiraAinda não há avaliações
- Type B (Hib) Vaccine: Haemophilus InfluenzaeDocumento2 páginasType B (Hib) Vaccine: Haemophilus InfluenzaeEnce MalatambanAinda não há avaliações
- Addison's Disease (Primary Adrenal Insufficiency)Documento5 páginasAddison's Disease (Primary Adrenal Insufficiency)sunnnydayAinda não há avaliações
- Chronic GastritisDocumento7 páginasChronic GastritisDivina AquinoAinda não há avaliações
- Teaching Case Presentation 2Documento20 páginasTeaching Case Presentation 2api-347034408Ainda não há avaliações
- Lab 5 Diabetes InsipidusDocumento6 páginasLab 5 Diabetes InsipidusLisa EkapratiwiAinda não há avaliações
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Thyroid CancerDocumento34 páginasThyroid CancerSahirAinda não há avaliações
- Acute Tonsillopharyngitis - NonexudativeDocumento12 páginasAcute Tonsillopharyngitis - NonexudativeLemuel GuevarraAinda não há avaliações
- Diabetes InsipidusDocumento7 páginasDiabetes Insipiduspaul_stefenson10Ainda não há avaliações
- Derma Case Write UpDocumento9 páginasDerma Case Write UpAmbhi GanaAinda não há avaliações
- Acute Lymphoblastic LeukemiaDocumento25 páginasAcute Lymphoblastic Leukemiaapi-396564080Ainda não há avaliações
- Aquino Typhoid Fever Case PresentationDocumento9 páginasAquino Typhoid Fever Case PresentationCalingalan Hussin CaluangAinda não há avaliações
- Final Hernioplasty Compilation RevisedDocumento58 páginasFinal Hernioplasty Compilation RevisedRaidis PangilinanAinda não há avaliações
- Dengue Case PresDocumento49 páginasDengue Case PresDee SarajanAinda não há avaliações
- Chronic GastritisDocumento37 páginasChronic GastritisBondu Babu007Ainda não há avaliações
- Rheumatic Heart DiseaseDocumento13 páginasRheumatic Heart Diseasedy15Ainda não há avaliações
- Angelic - Doc - Neonatal JaundiceDocumento16 páginasAngelic - Doc - Neonatal JaundiceAngy100% (5)
- Kaposi's SarcomaDocumento6 páginasKaposi's SarcomaveremkovichAinda não há avaliações
- Approach To HemoptysisDocumento22 páginasApproach To HemoptysisNikhil PanjiyarAinda não há avaliações
- Pathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsDocumento4 páginasPathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsLovely DaroleAinda não há avaliações
- Rectal CarcinomaDocumento16 páginasRectal Carcinomabuddy557Ainda não há avaliações
- Kidney Disorders 03.27.2019Documento33 páginasKidney Disorders 03.27.2019Emily EresumaAinda não há avaliações
- Food Challenge 03.20.2019Documento17 páginasFood Challenge 03.20.2019Emily EresumaAinda não há avaliações
- Ophtho Pearls 03.13.2019Documento17 páginasOphtho Pearls 03.13.2019Emily EresumaAinda não há avaliações
- Board Prep Metabolics Feb 2019Documento23 páginasBoard Prep Metabolics Feb 2019Emily EresumaAinda não há avaliações
- Dangers of Vaping 03.15.2019Documento23 páginasDangers of Vaping 03.15.2019Emily EresumaAinda não há avaliações
- Pediatric Hypertension Noon Conference 03.20.2019Documento44 páginasPediatric Hypertension Noon Conference 03.20.2019Emily EresumaAinda não há avaliações
- Morning Report Case Presentation: APRIL 1, 2019Documento14 páginasMorning Report Case Presentation: APRIL 1, 2019Emily EresumaAinda não há avaliações
- Investing 101 For Residents: RJ Nemeyer MDDocumento12 páginasInvesting 101 For Residents: RJ Nemeyer MDEmily EresumaAinda não há avaliações
- Case Presentation: Tad MiyaDocumento41 páginasCase Presentation: Tad MiyaEmily EresumaAinda não há avaliações
- Board Prep Genetics Dec 2018Documento62 páginasBoard Prep Genetics Dec 2018Emily EresumaAinda não há avaliações
- Tachycardia How To Keep Your Patient Alive in The Middle of The NightDocumento30 páginasTachycardia How To Keep Your Patient Alive in The Middle of The NightEmily Eresuma100% (1)
- Somatization 01.28.2019Documento28 páginasSomatization 01.28.2019Emily EresumaAinda não há avaliações
- Bells Palsy or Stroke 02.06.2019Documento19 páginasBells Palsy or Stroke 02.06.2019Emily EresumaAinda não há avaliações
- Board Prep GI Jan 2019Documento32 páginasBoard Prep GI Jan 2019Emily EresumaAinda não há avaliações
- Board Prep Emergency Ingestions Dec.2018Documento46 páginasBoard Prep Emergency Ingestions Dec.2018Emily EresumaAinda não há avaliações
- Chronic Granulomatous Disease 01.23.2019Documento10 páginasChronic Granulomatous Disease 01.23.2019Emily EresumaAinda não há avaliações
- Anemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentDocumento16 páginasAnemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentEmily EresumaAinda não há avaliações
- Morning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Documento24 páginasMorning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Emily EresumaAinda não há avaliações
- Ventilators 11.07.2018Documento38 páginasVentilators 11.07.2018Emily EresumaAinda não há avaliações
- Pertussis 01.14.2019Documento29 páginasPertussis 01.14.2019Emily EresumaAinda não há avaliações
- Morning Report: Melanie Nelson, PGY-2Documento25 páginasMorning Report: Melanie Nelson, PGY-2Emily EresumaAinda não há avaliações
- Wilderness Medicine 11.20.2018Documento12 páginasWilderness Medicine 11.20.2018Emily EresumaAinda não há avaliações
- Limping 12.10.2018Documento32 páginasLimping 12.10.2018Emily Eresuma100% (1)
- Jaundice 11.28.2018Documento13 páginasJaundice 11.28.2018Emily EresumaAinda não há avaliações
- Morning Report: Lindsey Gakenheimer-Smith MD PGY3Documento20 páginasMorning Report: Lindsey Gakenheimer-Smith MD PGY3Emily EresumaAinda não há avaliações
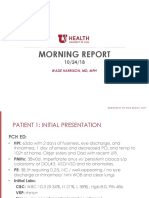
- Morning Report: Wade Harrison, MD, MPHDocumento13 páginasMorning Report: Wade Harrison, MD, MPHEmily EresumaAinda não há avaliações
- MysteryCase 10.22.18Documento10 páginasMysteryCase 10.22.18Emily EresumaAinda não há avaliações
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Documento35 páginasPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaAinda não há avaliações
- Halloween Safety: Dominique ChevalierDocumento21 páginasHalloween Safety: Dominique ChevalierEmily EresumaAinda não há avaliações
- Foster Care in Utah: Marlayna DespresDocumento11 páginasFoster Care in Utah: Marlayna DespresEmily EresumaAinda não há avaliações
- SESSION 13 Abnormal PsychologyDocumento47 páginasSESSION 13 Abnormal PsychologyKainaat YaseenAinda não há avaliações
- Low VisionDocumento7 páginasLow VisionUme HabibaAinda não há avaliações
- Diagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Documento8 páginasDiagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Fedrik Monte Kristo LimbongAinda não há avaliações
- Schizophrenia AmbossDocumento7 páginasSchizophrenia AmbossShrests SinhaAinda não há avaliações
- General Principles of Fracture ManagementDocumento60 páginasGeneral Principles of Fracture ManagementAdrian Joel Quispe AlataAinda não há avaliações
- XII - Zool Ch4 REPRODUCTIVE HEALTH Hsslive PDFDocumento4 páginasXII - Zool Ch4 REPRODUCTIVE HEALTH Hsslive PDFPrituAinda não há avaliações
- A Guide To The Pathology and Inspection of Poultry: H Thompson R Irvine D J Taylor W SteeleDocumento92 páginasA Guide To The Pathology and Inspection of Poultry: H Thompson R Irvine D J Taylor W SteeleorigatAinda não há avaliações
- OligohydramniosDocumento4 páginasOligohydramniossalamredAinda não há avaliações
- SOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticDocumento5 páginasSOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticvidyahamzahAinda não há avaliações
- Altamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Documento3 páginasAltamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Kanhaiya VermaAinda não há avaliações
- Visiting A DoctorDocumento12 páginasVisiting A DoctorНаталіяAinda não há avaliações
- DR Veronica Adetunji CVDocumento6 páginasDR Veronica Adetunji CVTobi OlanipekunAinda não há avaliações
- 17 - CIR V Philippine Health Care ProvidersDocumento2 páginas17 - CIR V Philippine Health Care ProvidersCamille AngelicaAinda não há avaliações
- Draft Examination Timetable For Msu Mid-Semester Examination, February 2016 SessionDocumento279 páginasDraft Examination Timetable For Msu Mid-Semester Examination, February 2016 SessionRebecca ChenAinda não há avaliações
- PTB Case-StudyDocumento64 páginasPTB Case-StudyBeverly DatuAinda não há avaliações
- Eating Disorders: by Pius KigamwaDocumento20 páginasEating Disorders: by Pius KigamwaRahul Kumar DiwakarAinda não há avaliações
- Hand Hygiene Audit March 19Documento17 páginasHand Hygiene Audit March 19Sammie WainainaAinda não há avaliações
- Thesis Plan FormatDocumento13 páginasThesis Plan FormatJotu ThakurAinda não há avaliações
- Protocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Documento17 páginasProtocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Sara Daoudi FuentesAinda não há avaliações
- Nursing Exam Questions 2023 Part 4Documento5 páginasNursing Exam Questions 2023 Part 4Lejo SunnyAinda não há avaliações
- Pleural Effusion: Etiology: Pleural Fluid Formation AbsorptionDocumento16 páginasPleural Effusion: Etiology: Pleural Fluid Formation AbsorptionitsireneAinda não há avaliações
- Rheumatology Handout - c2fDocumento1 páginaRheumatology Handout - c2fapi-195799092Ainda não há avaliações
- Clinical Avian Medicine - 2 Volume Set PDFDocumento1.057 páginasClinical Avian Medicine - 2 Volume Set PDFSilvana Martinez100% (3)
- NST and Their FunctionsDocumento5 páginasNST and Their FunctionsyazAinda não há avaliações
- Asiri Health Intermediate Care Centre: For Covid 19 Patients Siddhalepa Anarva Hotel A 4 Star, 100 Room FacilityDocumento3 páginasAsiri Health Intermediate Care Centre: For Covid 19 Patients Siddhalepa Anarva Hotel A 4 Star, 100 Room FacilityThilanka NiroshanaAinda não há avaliações
- SHD Form 4 T - NTPDocumento3 páginasSHD Form 4 T - NTPElle RochAinda não há avaliações
- C Reactive ProteinDocumento24 páginasC Reactive ProteinMohammed FareedAinda não há avaliações
- Firmalo, Eliazar M. Health Programs and Recommendations For Nong Pedro and FamilyDocumento2 páginasFirmalo, Eliazar M. Health Programs and Recommendations For Nong Pedro and FamilyEliazar FirmaloAinda não há avaliações
- Cranio SacralDocumento5 páginasCranio SacralIoan AndraAinda não há avaliações