Escolar Documentos
Profissional Documentos
Cultura Documentos
Morning Case Report: August 9th, 2014
Enviado por
hragunathan0 notas0% acharam este documento útil (0 voto)
11 visualizações23 páginasmorning report
Título original
MR
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentomorning report
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
11 visualizações23 páginasMorning Case Report: August 9th, 2014
Enviado por
hragunathanmorning report
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 23
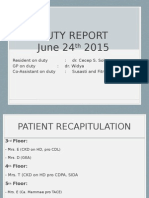
MORNING CASE REPORT
August 9th, 2014
PATIENT IDENTITY
Name (initial) : SSG
Sex : Male
Age : 46 years old
Religion : Hindu
Ethnic : Balinesse
Marital Status : Married
Address : Badung, Bali
Occupation : Wiraswasta
No. CM : 14046761
ToA : August 9
th
(14.30)
ANAMNESIS
Chief Complaint: Enlargement of the abdomen
Present History :
The patient complained of enlargement of abdomen
since 3 weeks BATH. The enlargement of his
abdomen was complained to have happened slowly
over time.
Patient complained of cough since 1 month ago
BATH. Initially, the cough was with no sputum and
recently 1 week BATH there was presence of sputum
in the cough.
Complain of fever was denied by the patient
There was shortness of breath complained 1 week
BATH along with the enlargement of the abdomen.
Anamnesis Cont.....
Passing of urine was normal with a frequency of 4-5
times per day, with a volume of 150-200cc each time.
There was no complain of vomiting blood.
But there was a complain of black stools 2 days BATH.
Past History
Patien was treated in RS Bakthi Rahayu for 19 days.
Patient was treated with Azithromycin and
Furosemide
Patient has a history of DM since 7 years ago.
Family History
None of his family members have similar
complaints.
History of DM (-), HT (-), respiratory ds (-), GI
ds (-), kidney ds (-)
Social History
The patient does not smoke or drink alcohol
Physical Examination
Present status:
General condition : moderately illness
Level of Consciousness : E4V5M6
VAS : 2
BP : 120/70 mmHg
Pulse rate : 88 bpm
Resp. rate : 23 bpm
Axillary temp. : 36,3
o
C
Weight : 52 kg
Height : 159 cm
BMI : 20,57 kg/m
2
PHYSICAL EXAMINATION
General Status
Eye : anemic -/-, icterus +/+, pupillary reflexes +/+ isocor, edema palpebrae -/-
ENT : Tonsil T1/T1 Normal, Pharing: hiperemis (-), gland swelling (-)
Neck : JVP PR +2 cm H
2
O, LN enlargement (-)
Thorax : symmetrical
Cor : Ins: ictus cordis unseen,
Pal : ictus cordis unpalpable
Per: UB : ICS 2
RB : right PSL
LB : ICS 5 MCL sinistra
Aus: S1S2 Single Regular, Murmur (-)
Lung: Ins : symetrical, spider naevi (-), ginekomastia (-)
Pal: VF N/N,
Per : sonor/sonor
Aus : ves +/+, wh-/-, rh -/-
PHYSICAL EXAMINATION
Abdomen : Ins: Dist (+), ascites (+)
Aus : Bowel sound (+) normal,
Pal : Liver/spleen unpalpable, murphys
sign (-),
Per : Tympany(+), flank pain -/-,
Extremeties :
Warm +/+, Edema -/-
+/+ -/-
LABORATORIES
Complete Blood Count
Parameter Result Unit Remarks Reference Range
WBC 17,30 10
3
/L High 4,1 10,9
-Ne 15,40 89,00% 10
3
/L 2,5 7,5
-Ly 1,19 6,80% 10
3
/L 1,0 4,0
-Mo 0,68 3,90% 10
3
/L 0,1 1,2
-Eo 0,00 0,04% 10
3
/L 0,0 0,5
-Ba 0,00 0,16% 10
3
/L 0,0 0,1
RBC 3,18 10
6
/L Low 4,00 5,20
HGB 10,1 g/dL Low 12,00 16,00
HCT 29,7 % Low 36,0 46,0
MCV 93,4 fL Low 80,0 100,0
MCH 31,7 pg 26,0 34,0
MCHC 34,9 g/dL 31,0 36,0
RDW 15,90 % High 11,60 14,80
PLT 499,00 10
3
/L High 150 440
LABORATORIES
Complete Blood Count
Parameter Result Unit Remarks Reference Range
MPV 9,3 fL 6,80 10,00
PT 15,60 second Normal = difference
with control < 2
seconds
INR 1,33 High 0,90 1,10
Control PT 13,50
APTT 29, 00 second Normal = difference
with control < 7
seconds
Control
APTT
34,70
LABORATORIES
Blood Chemistry
Parameter Result Unit Remarks Reference Range
SGOT 37,0 U/L High 11,00 - 27,00
SGPT 30,0 U/L 11,00 - 34,00
Total bilirubin 2,07 mg/dL High 0,30 1,10
Indirect bilirubin 0,43 mg/dL < 0,8
Direct bilirubin 1,639 mg/dL High 0,00 0,30
Protein total 7,23 g/dL 6,40 - 8,30
Albumin 2,248 g/dL Low 3,40 4,80
Globulin 4,982 g/dL High 3,20 3, 70
BUN 13,50 mg/dL 8,00 23,00
Creatinine 0,70 mg/dL 0,50 0,90
Random Blood Glukose 337,0 mg/dL High 70,00 140,00
LABORATORIES
Blood Chemistry
Parameter Result Unit Remarks Reference Range
Alkali Phospatase 96,89 U/L 42,00 -98,00
Gamma GT 38,92 U/L High 7,00 32,00
LABORATORIES
Blood Gas Analysis
Parameter Result Unit Remarks Reference Range
pH 7,47 High 7,35 7,45
pCO2 27,00 mmHg Low 35,00 45,00
pO2 91,00 mmHg 80,00 100,00
HCO3
-
19,70 mmol/L Low 22,00 26,00
TCO2 20,40 mmol/L Low 24,00 30,00
BEecf -4,00 mmol/L Low -2,00 2,00
SO2c 98,00 % 95,00 - 100,00
Na 127,00 mmol/L Low 136,00 145,00
K 5,70 mmol/L High 3,5 5,10
LABORATORIES
Urinalysis
Parameter Result Unit Remarks Reference Range
pH 5,00 5 - 8
Leucocyte 500 leu/uL +3 neg
Nitrite neg neg
Protein 25,00 +1 neg
Glucose 1.000 mg/dL +4 neg
Ketone 5,00 mg/dL +1 neg
Urobilinogen 4,00 mg/dL +2 neg
Bilirubin 3,00 mg/dL +2 neg
Erytrocyte 250,00 ery/uL +5 neg
Colour brown
pale yellow -
yellow
LABORATORIES
Urinalysis
Parameter Result Unit Remarks Reference Range
Sedimen urine:
- Leucocyte much /lp < 6/lp
- Eritrocyte much /lp < 3/lp
- Epitel - /lp
- Cillinder
granula cast
+
/lp
- Crystal amorph + /lp
- Bacteria + /lp
THORAX AP
- Cor : no enlargement
detected
- Pulmo : infiltrate in right
parahiler dan percardial.
- Right pleural sinus is sharp,
left is unevaluated.
- Right diaphragm is normal.
- Bones: no abnormalities found
BOF
-Increase in
distribution of
intestinal gas.
-no radio opaque region along the
urinary tract.
-Contour of kidney left and right is
unclear.
-psoas line of left and right is unclear.
-shadow of liver and spleen not seen
enlargement.
-there is osteophyte at VL 3,4,5 and the
intervetebral space is good.
ASSESSMENT
- Susp cirhosis hepatis
- Mild anemia ec susp iron deficiency anemia +
bleeding
- DM tipe II
THERAPHY
Hospitalized
IVFD NaCl 0,9 % 20 dpm
Oxygen mask 5 -6 l
NGT
Regular insulin drip 4 unit/hours untill BS 200 mg/dL, 2 unit/hours
untill BS < 200 mg/dL
PLANNING DIAGNOSIS
- FBS, BS 2 hours postprandial, HbA1c, lipid
profile
- USG
MONITORING
Vital sign
Complaints
Thank you....
Você também pode gostar
- Afternoon Report 9 April 2017Documento17 páginasAfternoon Report 9 April 2017Puteri Diah RahtiniAinda não há avaliações
- Morning Report Case: June 19, 2014Documento23 páginasMorning Report Case: June 19, 2014Sri DashinieAinda não há avaliações
- LeptospirosisDocumento19 páginasLeptospirosisFelicia adeline ChristianAinda não há avaliações
- Morning ReportDocumento17 páginasMorning ReportBanng BinggAinda não há avaliações
- Morning Report Case: MarchDocumento20 páginasMorning Report Case: Marchputri meiliawatiAinda não há avaliações
- Morning Report Case: Desember 15 TH 2016Documento15 páginasMorning Report Case: Desember 15 TH 2016Pramana AdiputraAinda não há avaliações
- Morning Report Case: 24 April, 2012Documento20 páginasMorning Report Case: 24 April, 2012Renata YolandaAinda não há avaliações
- Morning Report: Sunday, Oktober 7 2018Documento21 páginasMorning Report: Sunday, Oktober 7 2018Bhisma DewabrathaAinda não há avaliações
- Morning Report: 7 February 2011Documento20 páginasMorning Report: 7 February 2011adi_ancuxAinda não há avaliações
- Contoh Morning ReportDocumento23 páginasContoh Morning ReportDaondy Friarsa SoehartoAinda não há avaliações
- Morning Report: Thursday, November 15 2018Documento21 páginasMorning Report: Thursday, November 15 2018Lipo DuoAinda não há avaliações
- Morning Report Case: 16th July, 2012Documento18 páginasMorning Report Case: 16th July, 2012Felicia adeline ChristianAinda não há avaliações
- Morning Report Case: June 7, 2011Documento16 páginasMorning Report Case: June 7, 2011LittleChenaAinda não há avaliações
- Morning Report: Friday 20 April 2012Documento18 páginasMorning Report: Friday 20 April 2012Felicia adeline ChristianAinda não há avaliações
- Case Report COPDDocumento18 páginasCase Report COPDMia RisdayanthiAinda não há avaliações
- MR Interna Intoksikasi MetanolDocumento17 páginasMR Interna Intoksikasi Metanolvina_vermillionAinda não há avaliações
- POMR FIN CholangitisDocumento29 páginasPOMR FIN Cholangitisphyna27Ainda não há avaliações
- Morning Report Case: 7th October, 2011Documento29 páginasMorning Report Case: 7th October, 2011Felicia adeline ChristianAinda não há avaliações
- Morning Report Case: October 27, 2011Documento18 páginasMorning Report Case: October 27, 2011Biji OntaAinda não há avaliações
- MR 5 November 2018Documento16 páginasMR 5 November 2018BakingpancakesAinda não há avaliações
- Morning Report Case: June 18th, 2012Documento13 páginasMorning Report Case: June 18th, 2012Felicia adeline ChristianAinda não há avaliações
- MR IleusDocumento24 páginasMR IleusFelicia adeline ChristianAinda não há avaliações
- Morning Report 16 AprilDocumento10 páginasMorning Report 16 AprilFirdha RositaAinda não há avaliações
- MR GoutyDocumento25 páginasMR GoutyArvindan SubramaniamAinda não há avaliações
- Asma Bronkiale: Pembimbing: Prof. Dr. Dr. Tjok Raka Putra, SPPD-KRDocumento8 páginasAsma Bronkiale: Pembimbing: Prof. Dr. Dr. Tjok Raka Putra, SPPD-KRGustiAyuNindyaAinda não há avaliações
- SOS AYU - Ax - PeunjangDocumento11 páginasSOS AYU - Ax - PeunjangIka AyuAinda não há avaliações
- CHF Nyha III Ec. Alcoholic CardiomyopathyDocumento27 páginasCHF Nyha III Ec. Alcoholic CardiomyopathyAnonymous bC3Z8aAinda não há avaliações
- Case Report Case ReportDocumento18 páginasCase Report Case ReportMelly MirandaAinda não há avaliações
- Lapjag 10 Feb 2016 - AnemiaDocumento25 páginasLapjag 10 Feb 2016 - AnemiamyoganoAinda não há avaliações
- Afternoon Report: Thursday, July 1 2021 Case From Wednesday, June 30 2021Documento20 páginasAfternoon Report: Thursday, July 1 2021 Case From Wednesday, June 30 2021BakingpancakesAinda não há avaliações
- Crypt Orchid Is MDocumento29 páginasCrypt Orchid Is Mzackypradana95Ainda não há avaliações
- Duty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemDocumento15 páginasDuty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemGiovina FajarAinda não há avaliações
- MR Dhiarrea 10 September 2018Documento17 páginasMR Dhiarrea 10 September 2018GustiAyuNindyaAinda não há avaliações
- Morning Report Case: 16th July, 2012Documento20 páginasMorning Report Case: 16th July, 2012Felicia adeline ChristianAinda não há avaliações
- Morning Report Case: 17th Dec 2013Documento22 páginasMorning Report Case: 17th Dec 2013SunardiasihAinda não há avaliações
- Duty Report Er 23 07 2015Documento25 páginasDuty Report Er 23 07 2015Auditya WidyasariAinda não há avaliações
- MR DM Hematemesis IMADocumento15 páginasMR DM Hematemesis IMANadine BushAinda não há avaliações
- Lapag 28-04-2014Documento10 páginasLapag 28-04-2014ThieFeezaeAinda não há avaliações
- MR Belakang 24022021 RAM Ca Buli EDITDocumento25 páginasMR Belakang 24022021 RAM Ca Buli EDITWilujeng AnggrainiAinda não há avaliações
- Morning Report: June 2022 Physician in ChargeDocumento24 páginasMorning Report: June 2022 Physician in ChargeIka AyuAinda não há avaliações
- MR SipDocumento26 páginasMR SipFelicia adeline ChristianAinda não há avaliações
- Morning Report 6 AprilDocumento8 páginasMorning Report 6 AprilFirdha RositaAinda não há avaliações
- Case ReportDocumento34 páginasCase ReportMiftahul JannahAinda não há avaliações
- Mrs. Fera Febriyani/ 27 y.o/MR 1.43.51.17 Admitted On July 27 2019 at 11.00 PMDocumento11 páginasMrs. Fera Febriyani/ 27 y.o/MR 1.43.51.17 Admitted On July 27 2019 at 11.00 PMmonyet65Ainda não há avaliações
- POMR PakDhe R26HCU - NHL+Septic Condition+Febril Neutropenia+Hematoscezia - CINV+Anemi+Trombocytopenia+HypoalbuminDocumento42 páginasPOMR PakDhe R26HCU - NHL+Septic Condition+Febril Neutropenia+Hematoscezia - CINV+Anemi+Trombocytopenia+HypoalbuminPramudia DeniAinda não há avaliações
- Afternoon Report: 5 AUGUST 2017Documento14 páginasAfternoon Report: 5 AUGUST 2017Surya Saptono PutraAinda não há avaliações
- MR 190820 Dr. Haudhiya OkeDocumento53 páginasMR 190820 Dr. Haudhiya OkeRudy Arindra WijayaAinda não há avaliações
- CKD + Kejang SuyonoDocumento15 páginasCKD + Kejang Suyonodevi_pramulawatiAinda não há avaliações
- Ok - Cito 10 Agustus 2016 - PagiDocumento13 páginasOk - Cito 10 Agustus 2016 - PagiRilano UmbohAinda não há avaliações
- Morning Report Case: 18th July, 2012Documento19 páginasMorning Report Case: 18th July, 2012Felicia adeline ChristianAinda não há avaliações
- DHF (Amin)Documento19 páginasDHF (Amin)dewaayuindahAinda não há avaliações
- Morning ReportDocumento27 páginasMorning ReportDody PrasetyaAinda não há avaliações
- Nanda Hematemesis MelenaDocumento13 páginasNanda Hematemesis MelenaLiya AnjelinaAinda não há avaliações
- Infective EndocarditisDocumento8 páginasInfective EndocarditisAiman Arifin100% (1)
- Morning Report: Dr. Dikara WS Maulidy, SP - PDDocumento24 páginasMorning Report: Dr. Dikara WS Maulidy, SP - PDBethari Abi SafitriAinda não há avaliações
- Tn. SyaipudinDocumento13 páginasTn. SyaipudinRizki Valian AkbarAinda não há avaliações
- Duty Report On Ward 24-06-15Documento25 páginasDuty Report On Ward 24-06-15Annisa Rizki Ratih PratiwiAinda não há avaliações
- Case Based DiscussionDocumento49 páginasCase Based DiscussionMaulana IbrahimAinda não há avaliações
- Heteroanamnesa Chief Complaint: Coffe Ground Vomiting History of Present IllnessDocumento6 páginasHeteroanamnesa Chief Complaint: Coffe Ground Vomiting History of Present IllnessIka AyuAinda não há avaliações
- Nursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideNo EverandNursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideAinda não há avaliações
- BCS KardiovaskulerDocumento37 páginasBCS KardiovaskulerhragunathanAinda não há avaliações
- Rabies JournalDocumento2 páginasRabies JournalhragunathanAinda não há avaliações
- Primary Tumor (T) : All Anaplastic Carcinomas Are Considered Stage IVDocumento6 páginasPrimary Tumor (T) : All Anaplastic Carcinomas Are Considered Stage IVhragunathanAinda não há avaliações
- Rabies JournalDocumento2 páginasRabies JournalhragunathanAinda não há avaliações
- Pengaruh Volume Pemberian Air Terhadap Pertumbuhan Bibit Kelapa Sawit Di Pembibitan UtamaDocumento11 páginasPengaruh Volume Pemberian Air Terhadap Pertumbuhan Bibit Kelapa Sawit Di Pembibitan UtamaTahum MatfuahAinda não há avaliações
- Ficha Tecnica p501Documento4 páginasFicha Tecnica p501LizbethAinda não há avaliações
- Product Analysis Certificate: Propanol-2 (Iso-Propanol) A.RDocumento1 páginaProduct Analysis Certificate: Propanol-2 (Iso-Propanol) A.RAMMARAinda não há avaliações
- Turnitin Originality ReportDocumento20 páginasTurnitin Originality ReportNaomi Deirdre ReyesAinda não há avaliações
- Boiler Sizing Guide PDFDocumento1 páginaBoiler Sizing Guide PDFfmkhan21100% (1)
- HINO Dutro Fault Codes List PDFDocumento4 páginasHINO Dutro Fault Codes List PDFANH LÊAinda não há avaliações
- 1.8 CarderoDocumento29 páginas1.8 CarderoRodrigo Flores MdzAinda não há avaliações
- Stephane Moses The Angel of History Rosenzweig Benjamin Scholem PDFDocumento196 páginasStephane Moses The Angel of History Rosenzweig Benjamin Scholem PDFlivehuman100% (3)
- STPM Mathematics T Past Year Question P1 P2 P3Documento19 páginasSTPM Mathematics T Past Year Question P1 P2 P3Sou Voyage0% (3)
- Oscillations NotesDocumento48 páginasOscillations Notesabdulrehman881122Ainda não há avaliações
- 06 Brakes PDFDocumento6 páginas06 Brakes PDFAKILI PSIAinda não há avaliações
- Annual Report 2016Documento171 páginasAnnual Report 2016Angel GrilliAinda não há avaliações
- Inhalation AnestheticsDocumento27 páginasInhalation AnestheticsMarcelitaTaliaDuwiriAinda não há avaliações
- Green Revolution: It's Acheivements and FailuresDocumento24 páginasGreen Revolution: It's Acheivements and FailuresSingh HarmanAinda não há avaliações
- The Tenth House in AstrologyDocumento6 páginasThe Tenth House in AstrologytratakAinda não há avaliações
- How I Quit SmokingDocumento17 páginasHow I Quit Smokingquitsmoking100% (3)
- 12abmb2 Group4 Chapter1Documento20 páginas12abmb2 Group4 Chapter1Kenneth Del RosarioAinda não há avaliações
- The Symbols Found in TarotDocumento17 páginasThe Symbols Found in TarotPEdro100% (1)
- Allegheny Power Planning CriteriaDocumento19 páginasAllegheny Power Planning Criteriaksdp1Ainda não há avaliações
- Karunungang BayanDocumento6 páginasKarunungang BayanGeronimo DiazAinda não há avaliações
- GTE LAB MANUAL Ver 4 - 1Documento135 páginasGTE LAB MANUAL Ver 4 - 1akhilaAinda não há avaliações
- Description Features: PT6964 LED Driver ICDocumento15 páginasDescription Features: PT6964 LED Driver ICDhivya NAinda não há avaliações
- Metal-Tek Electric Contact Cleaner Spray - TDS (2021)Documento1 páginaMetal-Tek Electric Contact Cleaner Spray - TDS (2021)metal-tek asteAinda não há avaliações
- FPS Module 1Documento28 páginasFPS Module 1RickAinda não há avaliações
- Envgeo D 17 00052 - R1Documento42 páginasEnvgeo D 17 00052 - R1Recep AkanAinda não há avaliações
- Current Invoice No. 1: Enabling Works CeilingDocumento1 páginaCurrent Invoice No. 1: Enabling Works CeilingEyad RefaiAinda não há avaliações
- UD11T4107 English Maritime History Human FactorDocumento4 páginasUD11T4107 English Maritime History Human FactorParminder singh parmarAinda não há avaliações
- Introduction To Mass Transfer - Part 1Documento39 páginasIntroduction To Mass Transfer - Part 1Biniyam haile100% (1)
- S.No. Components Makes: 1 Grab Cranes - Gantry TypeDocumento4 páginasS.No. Components Makes: 1 Grab Cranes - Gantry TypeHarish KumarAinda não há avaliações
- 21 Century Mind ControlDocumento7 páginas21 Century Mind ControltrswartzAinda não há avaliações