Escolar Documentos
Profissional Documentos
Cultura Documentos
Medicare Settlements
Enviado por
John HentschelTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Medicare Settlements
Enviado por
John HentschelDireitos autorais:
Formatos disponíveis
2014 Livingston Law Firm Retreat
John C. Hentschel
February 1, 2014
One of the most completely impenetrable
texts within human experience.
Cooper University Hospital v. Sebelius, 636 F.3d
44, 45 (3d. Cir. 2010)
Medicare Basics
Reporting Obligations
Reimbursements for Paid Medical
Expenses
Set Asides for Future Expenses
Best Practices
Guaranteed health insurance
Works like regular private
market insurance
Premiums
Copays
Deductibles
Out of pocket costs
65 and over who worked and
paid into system
Younger disabled (SSD more
than 24 months)
End stage renal failure
ALS
Inpatient hospital stays
2 night rule
90 day maximum
SNF in some cirmcumstances
Hospice stays
Generally no monthly premium if
10 years of FICA payments
Monthly premium (deducted from
SS)
Out patient services after deductible
($147 in 2013)
Physician services
Diagnostic imaging
Tests
Durable medical equipment
Optional if still working and covered
under private insurance
Private health insurance funded through
beneficiary premiums plus private monthly
premium
Additional coverages
Reduced copays and deductibles
Anyone with Part A or Part B eligibility
Designed and administered through
private insurers and regulated through
CMS
In addition to traditional Part A/B
coverages
Separate premiums
If a personal injury plaintiff is Medicare
eligible, obligations and duties are
triggered for all involved in the action
Plaintiff
Defendants
Insurers
Health care providers
42 USC 1395y(b)(2) - Beneficiaries of GHP
who get payments from NGHP, i.e.
primary plans
Liability insurance
No-fault insurance (med pay)
Workers compensation
Self insurance
IF Medicare pays for an item or service
that should have been paid by a primary
plan, reimbursement required per 42
CFR 411.22.
See Overview of the Recovery Process
flowchart
Right of action for CMS against responsible
parties
Insurer or self-insurer
TPA
Employer
Facility or provider
Attorneys (US v. Harris 2009 U.S. Dist. LEXIS 23956
(N.D. W.Va. 2009))
Double damages plus interest
Private right of action
Does not apply to Medicare Advantage (Part C) Plans,
(Parra v. Pacificare of Arizona, Inc., 715 F.3d 1146 (9
th
Cir. 2012))
Who pays first if I have a claim for no-fault or liability insurance?
No-fault insurance or liability insurance pays first and Medicare pays
second, if appropriate.
If doctors or other providers are told you have a no-fault or liability
insurance claim, they must try to get paid from the insurance company
before billing Medicare. However, this may take a long time.
If the insurance company doesnt pay the claim promptly (usually within
120 days), your doctor or other provider may bill Medicare. Medicare
may make a conditional payment to pay the bill, and then later get back
any payments the primary payer should have made.
Medicare and Other Health Benefits: Your Guide to Who Pays First,
CMS, p. 13
Unlike most liens, no notice requirement
Super lien, i.e., superior to al other claims
Benficiary should notify COBC of the
availability of other coverages
COBC notifies recovery contractor
Contractor will Conditional Payment
Summary (CPS)
When settlement reached, demand letter
sent
Payment to CMS within 60 days
Plaintiffs counsel, since 1980, has had
the responsibility to report to CMS the
existence of other potential sources of
payment for medical services and items
Section 111 of MMSEA added new
reporting requirements
To have CMS pay appropriately for Medicare-covered items
and services furnished to Medicare beneficiaries.
Allows CMS to determine who should be the primary payer of
services.
Responsible Reporting Entities
Insurers
Liability insurance
Workers compensation
No fault
Self insured entities
Attorneys are NOT RREs
Identity of claimant
Individual filing claim directly against
applicable plan
Individual filing a claim against an individual
or entity insured or covered by the applicable
plan
Any other information required by CMS
(42 USC 1395y(b)(B)(ii))
DOB, ICD-9 Diagnosis, Payment amounts
See Quick Reference Guide
E-file
Secure web portal
Quarterly
Triggered by settlement with
beneficiary
Assuming ORM or paying TPOC
$1k/day for non-compliance
SMART Act of 2012 42 USC 1395y(b)(9)
In 2014, HHS will establish a minimum amount
below which reporting and reimbursement is not
required
Medicares interests must be settled before
any settlement funds distributed (42 USC
1392y(b)(8)(iii))
Process of identifying all payments can
take time and should be done prior to final
settlement discussions
RRE needs up to date CPS prior to
resolving case
If settlement will not satisfy all of plaintiffs
obligations
Holds offer open for a specified period of
time to allow plaintiff to attempt to
compromise amount owed CMS
See 42 CFR 411.37 re: reduction of amount due
to CMS for procurement costs
Specify how CMS paid
Medicare named a payee on settlement draft
Funds escrowed
Hold harmless and indemnity
Apportionment?
Waiver of private right of action
Reporting particulars
Set-Aside Arrangement An administrative
mechanism used to allocate a portion of a
settlement, judgment or award for future
medical and/or future prescription drug
expenses. A set-aside arrangement may be in
the form of a Workers Compensation
Medicare Set-Aside Arrangement (WCMSA),
No-Fault Liability Medicare Set-Aside
Arrangement (NFSA) or Liability Medicare Set-
Aside Arrangement (LMSA).
42 CFR 411.46 provides that if lump-sum
settlement is intended to provide for all
future medical expenses due to a work-
related injury, Medicare payments for such
services are excluded until the expenses
equal the amount of the payment
A fund of money set aside at the time of
the settlement that must be exhausted to
pay for injury related treatment before
Medicare can be used
Protects Medicares future interests
Formally reviewed by CMS
Provides safe harbor for beneficiary and WC
insurer
$25,000/$250,000 thresholds
See Reference Guide
No legal authority requiring their use
Hybrid cases?
Texas?
See May 25, 2011 Handout from Region VI
Practical problems
Liability considerations in settlement
No apportionment of future medical benefits
Potential uses
Life care plan
Special needs trust
Cannot on own decide to require a set
aside
Must rely on cooperation with beneficiary
In interest to do so to avoid
Double damages and interest
Easy target
Caveat beware of those trying to sell
services!
Identify early as practicable if a claimant is
a Medicare beneficiary
Even if no benefits paid, notice still must be given
Medical records
RRE queries
Communication with claims rep and client
on obligations and strategy for compliance
Special Interrogatories
Have YOU applied for or are YOU eligible for Medicare benefits ?
Please state the date on which YOU first became entitled to
receive such benefits.
Please state YOUR Health Insurance Claim Number.
Please state YOUR Social Security Number,
Are any of the medical expenses related to YOUR injuries been
submitted to, or paid by, Medicare?
Have you been diagnosed with Lou Gehrigs disease?
Are YOU receiving treatment for end-stage renal disease or
kidney failure?
Have YOU applied for SSDI (Social Security Disability) benefits?
If YOU have applied for SSDI, state the date of application and
the current status of your application.
Document Requests
All documents which refer, reflect or pertain to
communication with Medicare, CMS or any of its
contractors specifically including, but not limited
to, notice to COBC, Rights and Responsibility
letters, conditional payment letters (with payment
summary forms), and correspondence regarding
relatedness.
A photocopy of the front and back of YOUR
current Medicare card.
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Proving Medical Value Under HowellDocumento48 páginasProving Medical Value Under HowellJohn HentschelAinda não há avaliações
- WCAB Decision Re: Participation of Lien Holder Lien On Issue of Attorney's FeesDocumento8 páginasWCAB Decision Re: Participation of Lien Holder Lien On Issue of Attorney's FeesJohn HentschelAinda não há avaliações
- Acoem Releases Updated Position Paper On TheDocumento2 páginasAcoem Releases Updated Position Paper On TheJohn HentschelAinda não há avaliações
- Ault IADC Article-July 2011Documento11 páginasAult IADC Article-July 2011John HentschelAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Benefits Information - OptumRxDocumento5 páginasBenefits Information - OptumRxDoma PropertiesAinda não há avaliações
- Medical BillingDocumento229 páginasMedical BillingMohammad Apzar100% (6)
- Pharmacist (Haad/Doh) : Mahboob AliDocumento4 páginasPharmacist (Haad/Doh) : Mahboob AliMahboob AliAinda não há avaliações
- SMART Asthma TherapyDocumento4 páginasSMART Asthma TherapyKen Won100% (1)
- WBDG Hospitals & Care HomesDocumento394 páginasWBDG Hospitals & Care Homesaqua2376Ainda não há avaliações
- Covered Lives SummaryDocumento8 páginasCovered Lives Summarygaurav_johnAinda não há avaliações
- In-Patient Pharmacy Dispensing PersonnelDocumento3 páginasIn-Patient Pharmacy Dispensing Personneljanr123456Ainda não há avaliações
- Indian Pharmaceutical IndustryDocumento7 páginasIndian Pharmaceutical Industrykhem_singhAinda não há avaliações
- Austin AnaplastologyDocumento3 páginasAustin AnaplastologyAustin Publishing GroupAinda não há avaliações
- Running Head: Health Disparities 1 Erin Mcniel November 10, 2015 Kaplan University Health Disparities in The ElderlyDocumento5 páginasRunning Head: Health Disparities 1 Erin Mcniel November 10, 2015 Kaplan University Health Disparities in The ElderlyErinAinda não há avaliações
- Kakoloti - Key Issues Facing The Health Sector in The Next Five Years (2007)Documento19 páginasKakoloti - Key Issues Facing The Health Sector in The Next Five Years (2007)Dinesh PatelAinda não há avaliações
- Basics of Evaluation and ManagementDocumento45 páginasBasics of Evaluation and ManagementRoaring King100% (2)
- Cms 2567 05-13-08Documento41 páginasCms 2567 05-13-08jawtrey100% (3)
- 1Documento90 páginas1MARY ROSE ONGLEO DABOAinda não há avaliações
- UTSW Written Response To SettlementDocumento2 páginasUTSW Written Response To SettlementreesedunklinAinda não há avaliações
- FHIR and LOINCDocumento78 páginasFHIR and LOINCDaniel VreemanAinda não há avaliações
- Anitha Resume 2022Documento2 páginasAnitha Resume 2022syed ShadullahAinda não há avaliações
- Report On Educational Workshop OnDocumento3 páginasReport On Educational Workshop OnMakhanVermaAinda não há avaliações
- Ap - Licensure RN LPNDocumento20 páginasAp - Licensure RN LPNRonnel BenavidezAinda não há avaliações
- Blue Shield CA Employee Enrollment Template v20160101Documento8 páginasBlue Shield CA Employee Enrollment Template v20160101Anonymous RLktVcAinda não há avaliações
- Pecial Eature: Transitions in Pharmacy Practice, Part 3: Effecting Change-The Three-Ring CircusDocumento7 páginasPecial Eature: Transitions in Pharmacy Practice, Part 3: Effecting Change-The Three-Ring CircusSean BlackmerAinda não há avaliações
- Real Time 270/271 Payer List: Payer Name Payer ID NotesDocumento9 páginasReal Time 270/271 Payer List: Payer Name Payer ID NotesRam KumarAinda não há avaliações
- Ayushman Bharat Yojana: National Health Protection SchemeDocumento28 páginasAyushman Bharat Yojana: National Health Protection SchemeKailash NagarAinda não há avaliações
- American Health Care Act SummaryDocumento2 páginasAmerican Health Care Act SummaryStephen Loiaconi50% (2)
- 3 Definition and Prevalence of Dentofacial Deformities 2014 Orthognathic SurgeryDocumento8 páginas3 Definition and Prevalence of Dentofacial Deformities 2014 Orthognathic SurgeryiweourvgiuAinda não há avaliações
- GMHBA Cancellation FormDocumento1 páginaGMHBA Cancellation FormjikoljiAinda não há avaliações
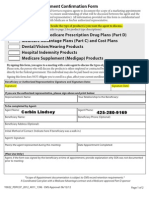
- 2013 Scope of Appointment Form - CORBINDocumento2 páginas2013 Scope of Appointment Form - CORBINCorbin LindseyAinda não há avaliações
- Health Care Reform Individual Insurance RequirementDocumento2 páginasHealth Care Reform Individual Insurance RequirementKimberly M MinetteAinda não há avaliações
- Florida Medicaid Pharmacy Claims AnalysisDocumento203 páginasFlorida Medicaid Pharmacy Claims AnalysisMatthew Daniel NyeAinda não há avaliações
- Delivery of Physical Therapy in The Acute Care Setting - A Population Based StudyDocumento17 páginasDelivery of Physical Therapy in The Acute Care Setting - A Population Based StudyCatalina EspiGaAinda não há avaliações