Escolar Documentos
Profissional Documentos
Cultura Documentos
Nursing Care Plan: Diagnosis
Enviado por
CharmaineTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Nursing Care Plan: Diagnosis
Enviado por
CharmaineDireitos autorais:
Formatos disponíveis
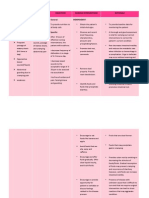
Nursing Care Plan
Diagnosis:
Risk for bleeding related to presence of
esophageal varices
Cues and
Clues
Nursing
Diagnosis
Scientific
Rationale
Objective Nursing Interventions Analysis Evaluation
Subjective:
The patient
verbalized
that she had
intermittent
bowel
movement
and vomiting
with blood.
Objective:
-
Hematemesis
- Melena
- EGD
findings:
Esophagus
varices grade
1-2 portal
hypertensive
gastropathy,
severe
Risk for
bleeding
related to
presence of
esophageal
varices
In portal
hypertension,
collateral
circulation
develops in
the lower
esophagus as
venous blood,
which is
diverted from
the GI tract
and spleen
because of
portal
obstruction,
seeks an
outlet.
At the end
of 1 hour of
nursing
intervention
, the patient
will
maintain
homeostasi
s with
absence of
bleeding
and
demonstrat
e
behaviours
to reduce
risk of
bleeding.
1. Provide an ongoing
assessment such as
ecchymosis, epistaxis,
petechiae, and
bleeding gums.
2. Monitor level of
consciousness, vital
signs, and urinary
output.
3. Encourage use of soft
toothbrush, electric
razor, avoiding
staining for stool,
forceful nose
blowing, and so forth.
1. To provide and
ensure
immediate
interventions
2. To evaluate
fluid balance
3. In the
presence of
clotting factor
disturbances,
minimal
trauma can
cause mucosal
bleeding.
At the end
of 1 hour of
nursing
intervention
, the patient
was able to
maintain
homeostasi
s with
absence of
bleeding
and
demonstrat
e
behaviours
to reduce
risk of
bleeding.
Because of
excessive
intraluminal
pressure, these
collateral veins
become
tortuous, dilated,
and fragile. They
are particularly
prone to
ulceration and
hemorrhage.
Rupture of
esophageal
varices is the
most common
cause of death of
clients with
hepatic cirrhosis.
4. Administer
medications
as indicated:
Supplementa
l vitamins
(e.g.,
Vitamins K,
D, and C);
Stool
softeners
5. Use small
needles for
injections.
Apply
pressure to
small
bleeding/ven
ipuncture
sites for
longer than
usual.
4. Promotes
prothromb
in
synthesis
and
coagulatio
n if liver is
functional.
Vitamin C
deficiencie
s increase
susceptibili
ty to
irritation/b
leeding
5. Minimizes
damage to
tissues,
reducing
risk of
bleeding/h
ematoma
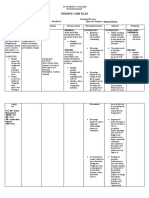
Fluid and Electrolyte Imbalance as
manifested in vomiting
Subjective:
Patient
verbalized
intermittent
vomiting and
bowel
movement
accompanied by
the presence of
blood.
Objective:
- Lab results:
Na 136mEq/L
K 3.54mEq/L
- Weak in
appearance
- Vomiting
- Diarrhea
Fluid and
Electrolyte
Imbalance as
manifested in
vomiting
The vomiting
reflex usually
causes a feeling
of nausea. The
vomiting center
in the medulla
sends signals
through the
body, which
starts a wave of
peristalsis in the
small intestine.
At the end of 1
hour of nursing
interventions,
the patient will
experience an
adequate fluid
volume and
electrolyte
balance as
evidenced by
urine output >
30mL per hour,
normal vital
signs,
consistency of
weight, and
normal skin
turgor.
1. Evaluate fluid
status in
relation to
dietary intake.
Determine if
patient has
been on a fluid
restriction.
2. Assess or
instruct patient
to monitor
weight daily
and
consistently,
with same
scale, and
preferably at
the same time
of day.
3. Monitor and
document vital
signs.
1. Most fluid
enters the body
through
drinking, water
in food, and
water formed
by oxidation of
food.
2. To facilitate
accurate
measurement
and follow
trends.
3. Sinus
tachycardia may
occur with
hypovolemia to
maintain an
effective cardiac
output. Usually
the pulse is
weak, and may
be irregular if
electrolyte
imbalance also
occurs.
At the end of 1
hour of nursing
interventions,
the patient was
able to
experience an
adequate fluid
volume and
electrolyte
balance as
evidenced by
urine output >
30mL per hour,
normal vital
signs,
consistency of
weight, and
normal skin
turgor.
Contractions
of the
stomach,
then
relaxation of
the stomach
increase
pressure and
forces gastric
and
intestinal
contents out
through the
esophagus
and mouth.
This causes
electrolyte
and fluid loss
because
these are
some of the
components
of the gastric
content
which are
lost
excessively.
4. Assess
skin turgor
and
mucous
membrane
s for signs
of
dehydratio
n.
5. Assess
color and
amount of
urine.
Report
urine
output less
than 30mL
per hour
for 2
consecutiv
e hours.
4. The skin
in elderly
patients
loses its
elasticity;
therefore
skin turgor
should be
assessed
over the
sternum or
on the
inner
thighs.
5.
Concentrat
ed urine
denotes
fluid
deficit.
Nutrition: imbalance, less than body
requirements
Subjective:
Patient
verbalized that
she vomited a lot
and this was
accompanied by
blood. She also
said that she
noticed a change
in her eating
habits because of
what happened.
Objective:
- Noted weakness
- Impaired
mobility and
ADLS by the use
of assistance
from relative
Nutrition:
imbalance,
less than
body
requireme
nts
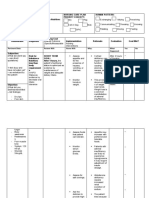
Metabolic
dysfunction in
the liver, such
as decreased
gluconeogenesi
s; decreased
bile for
digestion and
absorption;
portal
hypertension,
leading to
edema of
intestinal wall
and interfering
with digestion
and absorption
Short
term: At
the end of
1 hour of
nursing
interventi
on, the
patient
will
understan
d and
verbalize
the risk
factors
and self-
managem
ent in
gaining
proper
nutrition.
1. Weigh as
indicated.
Compare
changes in
fluid status,
recent
weight
history,
skinfold
measureme
nts.
2. Provide salt
substitutes,
if allowed;
avoid those
containing
ammonium.
1. It may be difficult to use
weight as a direct
indicator of nutritional
status in view of
edema/ascites. Skinfold
measurements are useful
in assessing changes in
muscle mass and
subcutaneous fat
reserves.
2. Salt substitutes enhance
the flavor of food and aid
in increasing appetite;
ammonia potentiates risk
of encephalopathy.
Short term: At
the end of 1 hour
of nursing
intervention, the
patient was able
to understand
and verbalize the
risk factors and
self-management
in gaining proper
nutrition.
Long term: At
the end of 5
hours of
nursing
intervention,
the patient
will
demonstrate
progressive
weight gain
toward goal
with patient-
appropriate
normalization
of laboratory
values and
experience no
further signs
of
malnutrition.
3. Restrict intake
of caffeine,
gas
producing or
spicy and
excessively
hot or cold
food.
4. Promote
undisturbed
rest periods,
especially
before
meals.
5. Provide tube
feedings,
TPN, liquids
as indicated.
3. Aids in reducing
gastric
irritation/diarrhe
a and abdominal
discomfort that
may impair oral
intake/digestion.
4. Conserving energy
reduces
metabolic
demands on the
liver and
promotes cellular
regeneration.
5. May be required to
supplement diet
or to provide
nutrients when
patient is too
nauseated or
anorexic to eat or
when esophageal
varices interfere
with oral intake.
Long term: At the
end of 5 hours of
nursing
intervention, the
patient was able
to demonstrate
progressive
weight gain
toward goal with
patient-
appropriate
normalization of
laboratory values
and experience
no further signs of
malnutrition.
Risk for Acute Confusion related to inability of
liver to detoxify certain enzymes or drugs
Subjective:
Patient
verbalized that
she is usually
forgetful and
she is having a
hard time
sleeping.
Objective:
- Bleeding
- Electrolyte
abnormalities
(hypokalemia
and
hyponatremia)
- GCS (4,4,6 =
14)
- insomnia
Risk for
Acute
Confusion
related to
inability of
liver to
detoxify
certain
enzymes or
drugs
Metaboli
c
dysfuncti
on with
inability
to
remove
ammonia
from
protein
metaboli
sm and
other
toxic
substanc
es
At the end of 1
hour of nursing
intervention, the
patient will
maintain usual
level of mentation
or reality
orientation and
initiate behaviours
or lifestyle changes
to prevent or
minimize
recurrence of
problem.
1. Review
current
medication
regimen/sc
hedules.
2. Evaluate
sleep/rest
schedule.
3. Maintain
bed rest,
assist with
self-care
activities.
1. Adverse drug
reactions or
interactions may
potentiate or
exacerbate
confusion.
2. Difficulty
falling/staying
asleep leads to
sleep deprivation,
resulting in
diminished
cognition and
lethargy.
3. Reduces
metabolic
demands on liver,
prevents fatigue,
and promotes
healing, lowering
risk of ammonia
buildup.
At the end of 1
hour of nursing
intervention,
the patient was
able to
maintain usual
level of
mentation or
reality
orientation and
initiate
behaviours or
lifestyle
changes to
prevent or
minimize
recurrence of
problem.
4. Reduce provocative
stimuli,
confrontation.
Refrain from
forcing activities.
Assess potential
for violent
behaviour.
5. Recommend
avoidance of
narcotics or
sedatives,
antianxiety agents,
and limiting or
restricting use of
medications
metabolized by the
liver.
4. Avoids triggering
agitation and
violent
responses;
promotes
patient safety.
5. Certain drugs are
toxic to the
liver, whereas
other drugs
may not be
metabolized
because of
cirrhosis,
causing
cumulative
effects that
affect
mentation,
mask signs of
developing
encephalopat
hy, or
precipitate
coma.
Risk for Impaired skin integrity related to
presence of edema
Subjective:
Minsan
namamana
s din ako,
as
verbalized
by the
patient.
Objective:
- Presence
of Liver
Cirrhosis
- Presence
of
hypertensio
n
- Warm
Skin
- Less
movement
or
flexibility
Risk for
Impaire
d skin
integrit
y
related
to
presenc
e of
edema
Due to
elevated
aldosteron
e and ADH
levels,
decreased
serum
albumin
levels
At the end
of 1 hour of
nursing
interventio
n, the
patient will
maintain
skin
integrity
and identify
individual
risk factors
and
demonstrat
e
behaviours/
techniques
to prevent
skin
breakdown.
1. Encourage/assi
st with
repositioning
on a regular
schedule,
while in
bed/chair, and
active/passive
ROM exercises
as appropriate.
2. Keep linens
dry and free of
wrinkles.
1. Repositioning
reduces
pressure on
edematous
tissues to
improve
circulation.
Exercises
enhance
circulation and
improve/mainta
in joint
mobility.
2. Moisture
aggravates
pruritus and
increases risk of
skin
breakdown.
At the end of 1 hour of
nursing intervention,
the patient was able to
maintain skin integrity
and identify individual
risk factors and
demonstrate
behaviours/techniques
to prevent skin
breakdown.
3. Use
alternating
pressure
mattress,
eggcrate
mattress,
waterbed,
sheepskins,
as indicated.
4. Restrict
sodium and
fluids as
indicated.
5. Provide
frequent
mouth care;
occasional ice
chips. (if
NPO)
3. Reduces dermal pressure,
increases circulation,
and diminishes risk of
tissue
ischemia/breakdown.
4. Sodium may be restricted
to minimize fluid
retention in
extravascular spaces.
Fluid restriction may be
necessary to
correct/prevent
dilutional hyponatremia.
5. Decreases sensation of
thirst
Você também pode gostar
- NCP AnemiaDocumento2 páginasNCP AnemiaAriaAinda não há avaliações
- Liver Cirrhosis Case PresDocumento77 páginasLiver Cirrhosis Case Presmarlx580% (5)
- Nursing Care PlanDocumento4 páginasNursing Care PlanJoy Callo100% (2)
- GMP History PDFDocumento49 páginasGMP History PDFSubhradipAinda não há avaliações
- Satir Theory Twenty Years After Her DeathDocumento4 páginasSatir Theory Twenty Years After Her DeathgoshAinda não há avaliações
- Site Logistics PlanDocumento2 páginasSite Logistics Plansampath_priyashantha75% (4)
- NCPDocumento3 páginasNCPWendy EscalanteAinda não há avaliações
- Liver Cirrhosis NCPDocumento21 páginasLiver Cirrhosis NCPJeco Valdez100% (4)
- Freight Loading and Unloading ProcedureDocumento4 páginasFreight Loading and Unloading ProceduretadchancAinda não há avaliações
- Nursing Care PlanDocumento4 páginasNursing Care PlanSharmaine Grace Florig100% (2)
- HSE Questionnaire - Dragon Oil. 2Documento10 páginasHSE Questionnaire - Dragon Oil. 2saneemlaltp thachaparamban0% (1)
- Cues Nursing DX Objectives Nursing Interventions RationaleDocumento5 páginasCues Nursing DX Objectives Nursing Interventions RationaleJamie IcabandiAinda não há avaliações
- Hypertension Nursing Care PlanDocumento3 páginasHypertension Nursing Care PlanAsylla PajijiAinda não há avaliações
- NCP - Anxiety Hypertension)Documento3 páginasNCP - Anxiety Hypertension)Jaja Jaime100% (2)
- Nursing Care Plan: General: Goals Met GenreralDocumento4 páginasNursing Care Plan: General: Goals Met GenreralRomzy Basañes100% (1)
- Leachables Best Practice Guideline Disposable Solutions For Biomanufacturing PDFDocumento36 páginasLeachables Best Practice Guideline Disposable Solutions For Biomanufacturing PDFAziz Aditya Wiguna100% (2)
- NCPDocumento2 páginasNCPJhel NabosAinda não há avaliações
- Ineffective Airway Clearance: Nursing Care PlanDocumento2 páginasIneffective Airway Clearance: Nursing Care PlanJose Mari F. Esguerra0% (1)
- NCP - Altered Tissue PerfusionDocumento2 páginasNCP - Altered Tissue PerfusionLeigh Kristel Andrion0% (1)
- Case: Liver Cirrhosis Assessment:: Nursing InferenceDocumento7 páginasCase: Liver Cirrhosis Assessment:: Nursing InferenceLovelyn GanirAinda não há avaliações
- NCP Acute Pain RT CancerDocumento3 páginasNCP Acute Pain RT CancerCharissa Magistrado De LeonAinda não há avaliações
- BioMedical Waste Management Issues ChallengesDocumento23 páginasBioMedical Waste Management Issues ChallengesArun Shree RAinda não há avaliações
- Case Study - Multiple SclerosisDocumento11 páginasCase Study - Multiple SclerosisMyrhaida BairullaAinda não há avaliações
- NCPsDocumento13 páginasNCPsRocel DevillesAinda não há avaliações
- OkhlaDocumento55 páginasOkhlaPoojit Popli50% (2)
- Gi-Rle - NCP For Deficient Fluid VolumeDocumento2 páginasGi-Rle - NCP For Deficient Fluid VolumeEvangeline Villa de Gracia100% (1)
- NCP Liver CirrhosisDocumento7 páginasNCP Liver CirrhosisIris Jimenez-BuanAinda não há avaliações
- Case Study of Children With Special NeedsDocumento21 páginasCase Study of Children With Special NeedsGrf Trust83% (69)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocumento3 páginasNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalAinda não há avaliações
- NCP CholelithiasisDocumento2 páginasNCP Cholelithiasiskmpg11100% (2)
- AnxolamDocumento38 páginasAnxolammanjitdeshmukh2Ainda não há avaliações
- Gallstone NCPDocumento2 páginasGallstone NCPKelly RiedingerAinda não há avaliações
- Free Health and Safety Action Plan TemplateDocumento4 páginasFree Health and Safety Action Plan TemplateAhmed M. RafatAinda não há avaliações
- Anima: Beyond Fantasy Character SheetDocumento4 páginasAnima: Beyond Fantasy Character SheetTristan TaksonAinda não há avaliações
- NCP Inffective Tissue PerfusionDocumento3 páginasNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCP HyperthermiaDocumento1 páginaNCP HyperthermiaLeo_Rabacca_3610100% (1)
- Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationsDocumento3 páginasAssessment Nursing Diagnosis Planning Interventions Rationale EvaluationsAjay SupanAinda não há avaliações
- NCP PancreatitisDocumento2 páginasNCP PancreatitisJeanelle Generoso100% (1)
- Glaucoma NCPDocumento4 páginasGlaucoma NCPChantal CaraganAinda não há avaliações
- NCP Chest PainDocumento2 páginasNCP Chest PainCG Patron BamboAinda não há avaliações
- NCP 2 Addison's DiseaseDocumento4 páginasNCP 2 Addison's DiseaseRenee RoSeAinda não há avaliações
- NCP Loss of AppetiteDocumento5 páginasNCP Loss of AppetiteStenneli Gumban Trojillo50% (2)
- NCP For RS-HF (Cor PulmonaleDocumento5 páginasNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- NCP - Acute PainDocumento1 páginaNCP - Acute PainjsthrAinda não há avaliações
- Body Weakness NCPDocumento1 páginaBody Weakness NCPtwicetrashAinda não há avaliações
- Nursing Care Plan Peptic UlcerDocumento3 páginasNursing Care Plan Peptic UlcerJefferson Baluyot PalmaAinda não há avaliações
- NCP DMDocumento6 páginasNCP DMstara123Ainda não há avaliações
- NCPDocumento7 páginasNCPJo Chiko FlorendoAinda não há avaliações
- NCP Imbalanced NutritionDocumento3 páginasNCP Imbalanced NutritionAav Canlas100% (1)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocumento3 páginasAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimAinda não há avaliações
- Subjective: IndependentDocumento6 páginasSubjective: IndependentLuvdonna BorresAinda não há avaliações
- Hyperthermia Pneumonia Nursing Care PlanDocumento1 páginaHyperthermia Pneumonia Nursing Care Planjustin_saneAinda não há avaliações
- NCP BPHDocumento8 páginasNCP BPHjyaba0% (1)
- NCP For ConcussionDocumento3 páginasNCP For Concussiontamtam_antonio100% (1)
- Diarrhea (AGE)Documento2 páginasDiarrhea (AGE)NursesLabs.com100% (1)
- NCP 2Documento2 páginasNCP 2Neil Abraham Mendoza Lalap100% (2)
- Carpenito-Moyet, L. J. (2009) : IndependentDocumento3 páginasCarpenito-Moyet, L. J. (2009) : IndependentClint DelacruzAinda não há avaliações
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocumento3 páginasSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaAinda não há avaliações
- CP Intestinal Obstruction Nursing Care PlanDocumento7 páginasCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaAinda não há avaliações
- Nursing Care Plan: Fluid Volume DeficitDocumento2 páginasNursing Care Plan: Fluid Volume DeficitGenEsis CarandangAinda não há avaliações
- Nursing Care PlanDocumento10 páginasNursing Care PlanZerica Andaca83% (6)
- Word Ncp.......... TetanusDocumento6 páginasWord Ncp.......... TetanusaianrAinda não há avaliações
- NCP For SVTDocumento6 páginasNCP For SVTRen VillenaAinda não há avaliações
- Nursing Care PlanDocumento4 páginasNursing Care PlanKath RubioAinda não há avaliações
- NCPDocumento7 páginasNCPChris Denver BancaleAinda não há avaliações
- NCPDocumento1 páginaNCPJachel Kathleen LaguioAinda não há avaliações
- Hypertension Nursing Care PlanDocumento1 páginaHypertension Nursing Care PlanSheila Mae Cabahug100% (1)
- Ncp-Impaired S.i.-NavidasDocumento4 páginasNcp-Impaired S.i.-NavidasFran LanAinda não há avaliações
- Hepatobiliary DisorderDocumento49 páginasHepatobiliary DisorderAhmed KanemazeAinda não há avaliações
- Diarrhea Nursing Diagnosis & Care Plans: in This ArticleDocumento12 páginasDiarrhea Nursing Diagnosis & Care Plans: in This ArticleZephas HillsAinda não há avaliações
- There Are Two Main Types of GastritisDocumento11 páginasThere Are Two Main Types of GastritisMike Faustino SolangonAinda não há avaliações
- PDF Document 5Documento28 páginasPDF Document 5Kirstin del CarmenAinda não há avaliações
- Case 034: ConstipationDocumento7 páginasCase 034: ConstipationZauza100% (1)
- SF2 - 2020 - Grade 6 - MALINISDocumento2 páginasSF2 - 2020 - Grade 6 - MALINISJerson S. SantiagoAinda não há avaliações
- Cardiovascular SystemDocumento11 páginasCardiovascular SystemBSN 2-2 Espiritu Melody Mae DAinda não há avaliações
- Rebeccas Resume Updated 7-2016Documento1 páginaRebeccas Resume Updated 7-2016api-498987425Ainda não há avaliações
- 7 Milk Leaflet EnglishDocumento4 páginas7 Milk Leaflet EnglishGilang ThmFscAinda não há avaliações
- Parkinsonism A General Motor Disability PDFDocumento9 páginasParkinsonism A General Motor Disability PDFRishabh SinghAinda não há avaliações
- ICCD Power Point 2015Documento16 páginasICCD Power Point 2015OhioOhioAinda não há avaliações
- Acknowledgment: Barangay San Jose, Sipalay CityDocumento5 páginasAcknowledgment: Barangay San Jose, Sipalay Cityracel joyce gemotoAinda não há avaliações
- How ERP Software by SAP Enabled ModernaDocumento3 páginasHow ERP Software by SAP Enabled ModernaMarie IriarteAinda não há avaliações
- 1 Bci-Horizon-Scan-Report-2021Documento72 páginas1 Bci-Horizon-Scan-Report-2021roberto210772Ainda não há avaliações
- Lab1ESR 08Documento11 páginasLab1ESR 08Muhamad AfidinAinda não há avaliações
- Vampires and Death in New England, 1784 To 1892Documento17 páginasVampires and Death in New England, 1784 To 1892Ferencz IozsefAinda não há avaliações
- CH 09Documento12 páginasCH 09Daniel DennyAinda não há avaliações
- Guide To Application For Registration of Medicinal Products - 4th EditiDocumento142 páginasGuide To Application For Registration of Medicinal Products - 4th EditiKdp03Ainda não há avaliações
- Experiment: Analysis of Milk: Output by Christian James MataDocumento2 páginasExperiment: Analysis of Milk: Output by Christian James MataSIJIAinda não há avaliações
- Method Development and Validation of RP-HPLCDocumento8 páginasMethod Development and Validation of RP-HPLCManuel PardiñaAinda não há avaliações
- National Political Parties in India: Hidayatullah National Law University Raipur, ChhattisgarhDocumento34 páginasNational Political Parties in India: Hidayatullah National Law University Raipur, ChhattisgarhshiviAinda não há avaliações
- ROTC ReviewerDocumento6 páginasROTC ReviewerJenelyn BorbonAinda não há avaliações