Escolar Documentos
Profissional Documentos
Cultura Documentos
Jurding THT Elva Handy
Enviado por
Handhy Tanara0 notas0% acharam este documento útil (0 voto)
7 visualizações32 páginasfwvsdsa
Título original
Ppt Jurding THT Elva Handy
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPTX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentofwvsdsa
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
7 visualizações32 páginasJurding THT Elva Handy
Enviado por
Handhy Tanarafwvsdsa
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
Você está na página 1de 32
JOURNAL READING
“Medical Management of Chronic Rhinosinusitis in Adults”
Pembimbing : dr. Khairan Irmansyah, Sp. THT-KL, M.Kes
ELVA OKTIANA RAHMI
HANDHY TANARA
1
Abstract
“ Chronic rhinosinusitis can be refractory and has
detrimental effects not only on symptoms, but
also on work absences, work productivity,
annual productivity costs, and disease-specific
quality of life measures.
There is evidence that it is driven by various
inflammatory pathways and host factors and is not
merely an infectious problem, although pathogens,
”
including bacterial biofilms, may certainly contribute to
this inflammatory cascade and to treatment resistance.
Given this, medical management should be
tailored to the specific comorbidities and problems in
an individual patient.
1. INTRODUCTION
Chronic rhinosinusitis affects all races to a significant extent.
Prevalence within the United States in one study was 13.8% in
African Americans, 13% in Caucasians, 8.8% in Hispanics, and 7%
in Asians
This emphasizes that chronic rhinosinusitis has a significant impact
on all ethnicities and has a large economic impact. This highlights
the importance of effective treatment.
2. Definition and Classification
Rhinosinusitis is defined as inflammation of the
paranasal sinuses and nasal cavity that causes
symptoms.
It may be classified as:
• Acute rhinosinusitis (ARS) when it lasts less than four
weeks’ duration
• Chronic rhinosinusitis (CRS) when it lasts more than
12 weeks. During this time, patients may have acute
exacerbations, superimposed on their chronic
rhinosinusitis.
Rhinosinusitis may be caused by viruses, bacteria,
fungi, and noninfectious causes.
3. Diagnosis and Assessment
Clinicians should assess for:
• Nasal obstruction
• facial pain/pressure/fullness
• purulent nasal discharge
• and hyposmia, with two or more symptoms for greater than 12
weeks being highly sensitive for CRS.
These symptoms are also nonspecific, it is also recommended
that patients have objective evidence of sinonasal inflammation,
which can be visualized during:
anterior rhinoscopy
nasal endoscopy
or on computed tomography.
Inflammation is documented when one visualizes:
• Purulent rhinorrhea or edema in the middle meatus or
anterior ethmoid region
• Polyps in the nasal cavity or middle meatus
• and/or radiographic findings of inflammation.
These findings and the patient’s symptoms should be
persistent for greater than 12 weeks despite adequate
treatment for ARS, in order to diagnose CRS.
In addition, clinicians should assess for other factors that may
affect treatment in CRS:
• the presence or absence of nasal polyps
• asthma
• cystic fibrosis
• ciliary dyskinesia
• and an immunocompromised state.
• One may also consider obtaining testing for allergy and
immune function
4. Treatment
4.1. Acute Exacerbations of CRS and Biofilms
It is widely accepted that acute exacerbations of CRS
should be treated with oral antibiotics and this is
recommended by American, European, and Canadian
guidelines/position papers.
It is well accepted that bacteria trigger ARS and there has
been concern that inadequately treated ARS could cause
CRS.
patients may have comorbidities affecting these patients’
symptoms that were not identified (i.e., allergies)
There is some evidence that bacterial biofilms and
bacteria within epithelial cells contribute to inflammatory
cascades
Biofilms including Streptococcus pneumonia, Haemophilus
influenzae, Moraxella catarrhalis, S. aureus, and Pseudomonas
aeruginosa have been commonly identified in CRS patients both with
and without nasal polyps.
In addition, patients with biofilms have more severe preoperative
sinus disease, persistence of postoperative symptoms after sinus
surgery, ongoing mucosal inflammation, and infections.
In general, empiric oral antibiotics are used to treat acute
exacerbations.
Empiric antibiotic coverage targets common bacteria found in
CRS: S. pneumonia, H. influenzae, M. catarrhalis, S. aureus, P.
aeruginosa, and anaerobes.
some effective options include:
amoxicillin-clavulanate
second or third generation cephalosporin
respiratory fluoroquinolones
4.2. Chronic Rhinosinusitis (CRS) with Nasal Polyps
There is a lot of evidence emerging that S. aureus is implicated in at
least a subset of patients with CRS with nasal polyps, because
colonizing staphylococcal bacteria are producing superantigenic
toxins (Sags) that increase eosinophilic inflammation and promote
the formation of nasal polyps.
Total eosinophil counts correlated with the presence of nasal polyps,
asthma, and aspirin intolerance
When nasal polyps are present in CRS, patients should be
treated with intranasal therapy, including topical
intranasal steroids and/or saline nasal irrigation for
symptomatic relief.
in addition to long-term management of the nasal polyps
themselves with intranasal glucocorticoids which
decrease polyp size, polyp recurrence, decrease nasal
symptoms, and improve nasal airflow.
Topical intranasal corticosteroids are more effective when
administered with correct technique.
Oral corticosteroids are effective in decreasing polyp size
and nasal symptoms in the short term, but this must be
balanced with the risks of oral corticosteroids. It may be
useful for planned short-term improvement.
Long-term oral macrolides may be beneficial because of
their anti-inflammatory effects.
Intranasal saline irrigation should be used, as opposed to
intranasal saline spray because of increased
effectiveness on symptom relief and improving quality of
life.
Endoscopic sinus surgery is safe and effective in patients
with CRS with nasal polyps and is typically recommended
when patients’ signs and symptoms are refractory to
medical therapy.
endoscopic sinus surgery was shown to have equivalent
efficacy to medical management
4.3. Chronic Rhinosinusitis without Nasal Polyps
Intranasal steroids and/or nasal saline irrigation have been
shown to be beneficial in CRS without nasal polyps with
improved symptom scores.
Additions to nasal saline irrigation that have shown benefit
include sodium hypochlorite 0.05% in patients with S. aureus,
this is also felt to have possible effects on P. aeruginosa
Using xylitol in water as a sinonasal irrigation improved
symptom control compared to saline irrigation and can
potentially be a useful adjunctive treatment
There is inadequate data to promote the use of oral steroids in
CRS without nasal polyps .
Topical antibiotics do not show benefit in CRS without nasal
polyps.
Long-term antibiotics, primarily macrolides (azithromycin 500 g
weekly or roxithromycin 150 g daily), have shown possible
therapeutic response after treatment for 12 weeks.
Endoscopic sinus surgery in CRS without nasal polyps has been
shown to be safe and effective when medical treatment has
failed
4.4. Allergy
Allergic rhinitis is present in 40%–84% of patients with CRS.
allergic rhinitis is a superimposed exacerbating factor of CRS.
Patients with allergies and CRS are also more symptomatic
than those that have CRS without allergic rhinitis, despite
similar CT findings.
Intranasal glucocorticoids and/or nasal irrigation can be
beneficial.
4.5. Asthma and Aspirin Sensitivity
There is a high prevalence of CRS in patients with asthma and
they have found that asthma severity directly correlates with
the severity of sinus disease on imaging.
When CRS is treated (medically or surgically), asthma
symptoms improve and the need for asthma medications
decreases
In aspirin-tolerant patients with asthma or allergic rhinitis,
leukotriene inhibitors that antagonize CYSLTR1 can be
potentially beneficial (montelukast and zafirlukast)
There has been a study that combined treatment with
intranasal fluticasone and montelukast correlated with
improvement of nasal polyp size and CT findings, in
addition to others that demonstrate montelukast is better
than placebo in CRS with nasal polyps.
In aspirin sensitive patients, aspirin avoidance is an
important part of the management plan. One may also
consider aspirin desensitization
4.6. Cystic Fibrosis (CF)
CRS is reported in 30 to 67% of patients with CF (within all
age groups)
Some studies have suggested that this may be because
of genetic mutation.
It is clearer that similar bacteria occupy the upper and
lower airways of these CF patients, suggesting a
possible spread from the upper to lower airways
Inflammatory pathways may be treatment targets, in addition to
gene therapy and treatment of their microbiology.
More aggressive combined medical and surgical treatment
demonstrates improved control of CRS in CF patients.
A mucolytic, dornase alfa, once daily (2.5 mg)
administered intranasally either one month after
endoscopic sinus surgery, or without surgery
has been found to be improve compared to hypotonic
saline or normal saline.
It is also used for lower airway disease in these patients, but
with different dosing regimens and administration route (oral
inhalation).
topical antimicrobials show that they should not be first-
line therapies in CF patients for CRS.
There was a case report of successful use of ivacaftor in
refractory CRS related CF gene defect. Ivacaftor, a CF
transmembrane conductance regulator (CFTR)
potentiator, targets the G55ID-CFTR mutation in CF.
patients with CF that have endoscopic sinus surgery with
serial antimicrobial lavage had better outcomes than
surgery alone
4.7. Ciliary Dyskinesia
Decreased mucociliary clearance from ciliary dyskinesia
impacts a small percentage of patients with CRS (aside from
CF). Mucociliary transit time (MTT) is prolonged when patients
have underlying genetic-related ciliary dyskinesia
Effective treatments need to be further elucidated.
4.8. Immunodeficiency
Treatment with intravenous immunoglobulins (IVIG) and/or
prophylactic antibiotics is indicated in those with
immunoglobulin deficiency, which can improve survival
and decrease life-threatening infections.
However, it does not appear to affect radiologic
appearance of CRS and it is unclear that this clinically
improves CRS. Those with immunosuppression from HIV
infection should be treated for HIV to raise their CD4 count.
4.9. Fungal
Fungi have been found to be prevalent in patients with CRS
and local nasal tissue samples exhibit increased eosinophils,
but without increased IgE to indicate a mold allergy.
It is recommended not to use oral or topical antifungals given
greater risk of harm over potential benefit, in addition to their
high cost.
One area that remains less clear is allergic fungal
rhinosinusitis which appears to be a clinically distinct entity. It
demonstrates a Th2 immune response and also has specific
IgE in eosinophilic mucin and mucosa.
Treatment impact of this needs to be further elucidated.
Surgery with and without concomitant medical
management has been beneficial in allergic fungal
rhinosinusitis
CONCLUSIONS
• Chronic rhinosinusitis presents with uniform signs and
symptoms, but should be medically managed
according to the medical comorbidities and clinical
features present in an individual patient.
“I believe that the greatest gift you can
give your family and the world is a healthy
you”
- Joyce Meyer
THANKYOU
Você também pode gostar
- Delusional Disorder MedscapeDocumento14 páginasDelusional Disorder MedscapeHandhy Tanara100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
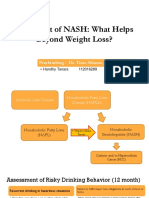
- Jurnal NashDocumento17 páginasJurnal NashHandhy TanaraAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Physiology of Bleeding To DeathDocumento2 páginasThe Physiology of Bleeding To DeathHandhy TanaraAinda não há avaliações
- Pertanyaan IleusDocumento1 páginaPertanyaan IleusHandhy TanaraAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Jurnal Reading: Treatment of NASH: What Helps Beyond Weight Loss?Documento1 páginaJurnal Reading: Treatment of NASH: What Helps Beyond Weight Loss?Handhy TanaraAinda não há avaliações
- Sharoon Covid TestDocumento3 páginasSharoon Covid TestVande GuruParamparaAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- NICU Manual Cheat SheetDocumento2 páginasNICU Manual Cheat Sheetlori_quintal92% (13)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Ocular Allergy Esen Karamursel Akpek, MDDocumento8 páginasOcular Allergy Esen Karamursel Akpek, MDAndri SaputraAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Etiology - The Etiology of Psoriasis Is ADocumento2 páginasEtiology - The Etiology of Psoriasis Is AJake DukesAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Vaccine Rejection and HesitancyDocumento7 páginasVaccine Rejection and HesitancyAlexander FrischAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- CHECKLIST PROCEDURES (Immunization)Documento2 páginasCHECKLIST PROCEDURES (Immunization)Elaine Frances IlloAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Elecsys Hbsag Ii: A) Tris (2,2'-Bipyridyl) Ruthenium (Ii) - Complex (Ru (Bpy) )Documento5 páginasElecsys Hbsag Ii: A) Tris (2,2'-Bipyridyl) Ruthenium (Ii) - Complex (Ru (Bpy) )Brian SamanyaAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Concept Mapping: Hodgskin'S Disease ComplicationDocumento4 páginasConcept Mapping: Hodgskin'S Disease ComplicationAsterlyn ConiendoAinda não há avaliações
- Acute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Documento35 páginasAcute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Tarik PlojovicAinda não há avaliações
- Nuñal Group - THYPHOID FEVER DraftDocumento5 páginasNuñal Group - THYPHOID FEVER Draftvirgo paigeAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Hospital Infection ControlDocumento31 páginasHospital Infection ControlIndian Railways Knowledge PortalAinda não há avaliações
- Anaphy Lec Sas-17Documento4 páginasAnaphy Lec Sas-17Francis Steve RipdosAinda não há avaliações
- In Defence of Self - How The Immune System Really Works (Oxford, 2007)Documento276 páginasIn Defence of Self - How The Immune System Really Works (Oxford, 2007)Crina Cryna100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- WHO Guide For Rabies Prevention Strategy. Updated 2018Documento12 páginasWHO Guide For Rabies Prevention Strategy. Updated 2018candida samAinda não há avaliações
- Study The Following Case. Fill in The Blanks With The Correct To BeDocumento3 páginasStudy The Following Case. Fill in The Blanks With The Correct To BeAnggita Heryani FIKA 2CAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Catalogo Web General ENDocumento9 páginasCatalogo Web General ENmrashrafiAinda não há avaliações
- Neonatal InfectionsDocumento18 páginasNeonatal InfectionsSanthosh.S.U100% (1)
- B.B Immunology For Blood BankDocumento26 páginasB.B Immunology For Blood BankAbode AlharbiAinda não há avaliações
- Meningitis PDFDocumento8 páginasMeningitis PDFrizeviAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- VPD Report 2019 MayDocumento12 páginasVPD Report 2019 MaystprepsAinda não há avaliações
- REGENERATE - How To Reverse COVID Vaxx Related Injuries and Repair Damaged TissueDocumento46 páginasREGENERATE - How To Reverse COVID Vaxx Related Injuries and Repair Damaged TissuemihailuicanAinda não há avaliações
- Newly Diagnosed HIV Cases in The Philippines: National Epidemiology CenterDocumento4 páginasNewly Diagnosed HIV Cases in The Philippines: National Epidemiology CenterDeden DavidAinda não há avaliações
- Blood Transfusion Policy 6.3Documento90 páginasBlood Transfusion Policy 6.3raAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Introduction To ImmunologyDocumento10 páginasIntroduction To ImmunologyArvi MandaweAinda não há avaliações
- Internal MedicineDocumento277 páginasInternal MedicineAhmad Abu ArkoubAinda não há avaliações
- Tuberculosis PowerpointDocumento69 páginasTuberculosis PowerpointCeline Villo100% (1)
- Subcutaneous MycosesDocumento16 páginasSubcutaneous MycosesMohamedAinda não há avaliações
- Hemorrhagic FeverDocumento3 páginasHemorrhagic FeverDenis QosjaAinda não há avaliações
- Prevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaDocumento8 páginasPrevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaUMYU Journal of Microbiology Research (UJMR)Ainda não há avaliações
- Journa L Read ING: Reta Fit Riana Ku Suma 01.211. 6497Documento29 páginasJourna L Read ING: Reta Fit Riana Ku Suma 01.211. 6497Ricky ZafiriantoAinda não há avaliações