Escolar Documentos
Profissional Documentos
Cultura Documentos
Hymodynamic Monitoring
Enviado por
Manesa ManeshaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Hymodynamic Monitoring
Enviado por
Manesa ManeshaDireitos autorais:
Formatos disponíveis
Chapter 9
Hemodynamic Monitoring
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Indications for Hemodynamic Monitoring
• Assesses cardiac function and evaluates effectiveness of
therapy
– Cardiogenic shock
– Severe heart failure
– Sepsis or septic shock
– Multiple organ system dysfunction (MODS)
– Acute respiratory distress syndrome (ARDS)
– Cardiac surgery
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
System Components
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
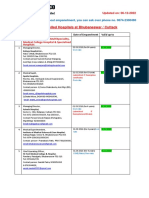
Square-Wave Test
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Leveling and Zeroing
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• To ensure accurate arterial pressures, the nurse must
level the transducer to what landmark?
– A. Nipple line
– B. Phlebostatic axis
– C. Sternal notch
– D. Apical impulse
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• B. Phlebostatic axis
• Rationale: The phlebostatic axis is between the fourth
intercostal space and midaxillary line; this is the
approximate location of the right atrium.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Arterial Pressure Monitoring
• Continuous monitoring of arterial blood pressure
• Vascular access for obtaining blood samples
• Guides therapy
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Interventions for Arterial Lines
• Ensure insertion site is visible at all times.
• Ensure monitor alarms are visible and audible.
• Set parameters according to the facility protocol.
– Typically 10 to 20 mm Hg of the patient’s trended
blood pressure
• DO NOT infuse IV solution or medication through the
arterial pressure monitoring system.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Data Interpretation
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• Is the following question True or False?
• It is acceptable to infuse medications via an arterial line.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• False
• Rationale: An arterial pressure line is used for monitoring
purposes only. NEVER infuse any medications or IV
solutions via this line.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Arterial Lines
• Accidental blood loss
– Secure and tighten connections.
– Immobilize extremity.
– Expose extremity.
• Infection
– Observe a sterile technique.
– Maintain a closed system.
• Impaired circulation
– Assess color, sensation, temperature, and movement
of extremity.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Central Venous Pressure Monitoring
• Normal values 2 to 8 mm Hg
• Measures right atrial pressure
• Left ventricular end-diastolic pressure
• Reflects intravascular blood volume
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Central Venous Catheters
• Infection
– Assess the site.
– Observe a sterile technique with any catheter
manipulation.
• Thrombosis
– Monitor waveform, ability to flush, blood return.
• Pneumothorax
– CXR postinsertion
• Air embolism
– Ensure tight connections.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• Is the following statement True or False?
• A central venous catheter measures right atrial pressure,
left ventricular end-diastolic pressure, and intravascular
blood volume.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• True
• Rationale: Central venous catheter terminates in the
superior vena cava near the right atrium; it measures
right atrial pressures, left ventricular end-diastolic
pressure, and intravascular blood volume.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pulmonary Artery Catheter
• Four lumens
– Distal lumen
– Proximal lumen
– Thermistor lumen
– Balloon inflation lumen
*Some PACs may have additional lumens.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Interventions for Pulmonary
Artery Catheters
• Assist with insertion.
• Monitor waveform.
• Observe for dysrhythmias.
• Observe for accidental wedging of the catheter.
• Maintain sterile dressing.
*Central catheter placement must be confirmed by CXR
before accessing the device.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Data Interpretation
• Right atrial pressure 2 to 6 mm Hg
– Measures pressure in the right ventricle during
diastole, equals CVP
• Right ventricular pressure 20 to 30 mm Hg
– Equals the pulmonary artery systolic pressure
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Data Interpretation (cont.)
• Pulmonary artery pressure
– Systolic pressure equals right ventricular systolic
function 20 to 30 mm Hg.
– Diastolic pressure equals the left ventricular end-
diastolic pressure (LVEDP) 8 to 15 mm Hg.
• Pulmonary artery wedge pressure 8 to 12 mm Hg
– More accurate measure of LVEDP
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Complications of Pulmonary Artery
Catheters
• Ventricular dysrhythmias
• Pulmonary artery rupture or perforation
• Pulmonary infarction
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cardiac Output
• Cardiac output (CO)—the amount of blood ejected from
the heart per minute
• Stroke volume (SV)—the milliliters of blood ejected from
the ventricle with each contraction
• HR x SV=CO
• 4 to 8L/minute at rest
• Cardiac index (CI)—relates cardiac output to body size;
normal is 2.5 to 4L/minute/m2.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Stroke Volume
• Preload
– Amount of stretch on the myocardial muscle fibers at
end diastole
• Afterload
– The resistance to ejection of blood from the
ventricles
• Contractility
– Ability of the heart to contract independent of
preload and afterload
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Methods of Evaluating Cardiac Output
• Thermodilution
• Arterial pressure and waveform-based methods
• Electrical bioimpedance cardiography
• Esophageal Doppler monitoring
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• Determinants of stroke volume includes all of the
following except what?
– A. Preload
– B. Cardiac output
– C. Afterload
– D. Contractility
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• B. Cardiac output
• Rationale: Stroke volume is the volume of blood ejected
from the ventricle with each contraction. Preload,
afterload, and contractility determine stroke volume.
Stroke volume X heart rate = cardiac output
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Thermodilution Technique
• Gold standard for evaluating cardiac output
– Intermittent
• Measures change in blood temperature following
injection of indicator solution
– Continuous
• Specialized PACs with thermal filaments
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Thermodilution Technique (cont.)
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cardiac Output Curves
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Thermodilution Technique (cont.)
• Ensure volume of injectate in the syringe is correct.
• Inject the volume smoothly and rapidly, less than 4
seconds.
• Wait approximately 1 minute between injections to allow
the catheter thermistor to return to baseline.
• Obtain three or more consecutive measurements.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Arterial Pressure and Waveform-Based
Method
• Proportional relationship between pulse pressure and
stroke volume
• Inverse relationship between pulse pressure and aortic
compliance
• Measures using an arterial line, special sensor, and a
monitor that uses an algorithm for SV and CO
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Impedance Cardiography
• Electrodes placed on the base of the neck and lower
thorax
• Measures impedance over time and is mathematically
converted into SV and CO values using an algorithm
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Esophageal Doppler Monitoring
• Doppler transducer in nasogastric tube
• Placed in esophagus and monitors blood flow velocity
through the descending aorta
• Continuous CO and SV are calculated using an algorithm.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• What is the most widely used method to determine
cardiac output?
– A. Arterial pressure and waveform method
– B. Impedance cardiography
– C. Esophageal Doppler monitoring
– D. Thermodilution
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• D. Thermodilution
• Rationale: Thermodilution is the most common method
used to measure cardiac output and is considered the
clinical gold standard.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Oxygen Delivery and
Demand Balance
• Oxygen delivery (DaO2)
– Amount of oxygen transported to tissues
– Depends on cardiac output, hemoglobin levels, and
arterial oxygen saturation
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Balance Between Supply and Demand
• Oxygen consumption—the amount of oxygen used by the
cells of the body
• Primary determinants:
– Oxygen demand—the cells requirement for oxygen
– Oxygen delivery—need adequate supply of oxygen to
deliver to the cells
– Oxygen extraction—the amount of oxygen removed
from Hgb to be used by the cells
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Global Tissue Oxygenation
Status
• Metabolic indicators
– Lactate levels, serum pH, and base excess/base
deficit
• Venous oxygen saturation
– Evaluates oxygen supply versus oxygen demand
– Mixed venous oxygen saturation SvO2
– Venous oxygen saturation ScvO2
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question
• Is the following statement True or False?
• Oxygen extraction is the amount of oxygen removed
from Hgb to be used by the cells.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer
• True
• Rationale: Oxygen extraction—the amount of oxygen
removed from Hgb to be used by the cells; oxygen
demand is the cells’ requirement for oxygen, oxygen
delivery the need for adequate supply of oxygen to
deliver to the cells.
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors Affecting Oxygen Supply Versus
Demand
• Surgery • Sepsis
• Infection • Anesthesia
• Pain • Suctioning
• Hypothermia • Pharmacological
paralysis
• Sedation
• Anxiety
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Evaluation of Regional Tissue
Oxygenation Status
• Gastric tonometry
– Specialized nasogastric tube measures partial
pressure of carbon dioxide (PCO2)
• Sublingual capnometry
– Measures PCO2 under the tongue
Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Corporate Tax Planning AY 2020-21 Sem V B.ComH - Naveen MittalDocumento76 páginasCorporate Tax Planning AY 2020-21 Sem V B.ComH - Naveen MittalNidhi LathAinda não há avaliações
- Case No. Class Action Complaint Jury Trial DemandedDocumento43 páginasCase No. Class Action Complaint Jury Trial DemandedPolygondotcom50% (2)
- 3g Node B On Ip MediaDocumento79 páginas3g Node B On Ip MediaBsskkd KkdAinda não há avaliações
- Flowrox Valve Solutions Catalogue E-VersionDocumento16 páginasFlowrox Valve Solutions Catalogue E-Versionjavier alvarezAinda não há avaliações
- Perturbation MethodsDocumento29 páginasPerturbation Methodsmhdr100% (1)
- Watch One Piece English SubDub Online Free On Zoro - ToDocumento1 páginaWatch One Piece English SubDub Online Free On Zoro - ToSadeusuAinda não há avaliações
- BA 4722 Marketing Strategy SyllabusDocumento6 páginasBA 4722 Marketing Strategy SyllabusSri GunawanAinda não há avaliações
- Chestionar 2Documento5 páginasChestionar 2Alex AndruAinda não há avaliações
- Sanskrit Lessons: �丘��恆� � by Bhikshuni Heng HsienDocumento4 páginasSanskrit Lessons: �丘��恆� � by Bhikshuni Heng HsiendysphunctionalAinda não há avaliações
- Jurnal 1 Ieevee LPF PDFDocumento4 páginasJurnal 1 Ieevee LPF PDFNanda SalsabilaAinda não há avaliações
- Marieb ch3dDocumento20 páginasMarieb ch3dapi-229554503Ainda não há avaliações
- Gmail - ICICI BANK I PROCESS HIRING FOR BACKEND - OPERATION PDFDocumento2 páginasGmail - ICICI BANK I PROCESS HIRING FOR BACKEND - OPERATION PDFDeepankar ChoudhuryAinda não há avaliações
- Nyamango Site Meeting 9 ReportDocumento18 páginasNyamango Site Meeting 9 ReportMbayo David GodfreyAinda não há avaliações
- Controlled DemolitionDocumento3 páginasControlled DemolitionJim FrancoAinda não há avaliações
- Laudon - Mis16 - PPT - ch11 - KL - CE (Updated Content For 2021) - Managing Knowledge and Artificial IntelligenceDocumento45 páginasLaudon - Mis16 - PPT - ch11 - KL - CE (Updated Content For 2021) - Managing Knowledge and Artificial IntelligenceSandaru RathnayakeAinda não há avaliações
- Bulletin PDFDocumento2 páginasBulletin PDFEric LitkeAinda não há avaliações
- A Brief Tutorial On Interval Type-2 Fuzzy Sets and SystemsDocumento10 páginasA Brief Tutorial On Interval Type-2 Fuzzy Sets and SystemstarekeeeAinda não há avaliações
- A Process Reference Model For Claims Management in Construction Supply Chains The Contractors PerspectiveDocumento20 páginasA Process Reference Model For Claims Management in Construction Supply Chains The Contractors Perspectivejadal khanAinda não há avaliações
- 2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFDocumento18 páginas2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFsantoshiAinda não há avaliações
- MN Rules Chapter 5208 DLIDocumento24 páginasMN Rules Chapter 5208 DLIMichael DoyleAinda não há avaliações
- Zambia National FormularlyDocumento188 páginasZambia National FormularlyAngetile Kasanga100% (1)
- Fluoride - Wide Range of Serious Health Problems"Documento29 páginasFluoride - Wide Range of Serious Health Problems"zataullah100% (2)
- Barista Skills Foundation Curriculum enDocumento4 páginasBarista Skills Foundation Curriculum enCezara CarteșAinda não há avaliações
- Channel & Lomolino 2000 Ranges and ExtinctionDocumento3 páginasChannel & Lomolino 2000 Ranges and ExtinctionKellyta RodriguezAinda não há avaliações
- Parker HPD Product Bulletin (HY28-2673-01)Documento162 páginasParker HPD Product Bulletin (HY28-2673-01)helden50229881Ainda não há avaliações
- Beautiful SpotsDocumento2 páginasBeautiful SpotsLouise Yongco100% (1)
- D. Das and S. Doniach - Existence of A Bose Metal at T 0Documento15 páginasD. Das and S. Doniach - Existence of A Bose Metal at T 0ImaxSWAinda não há avaliações
- Economizer DesignDocumento2 páginasEconomizer Designandremalta09100% (4)
- Plant Report Template Class 81Documento2 páginasPlant Report Template Class 81Kamran KhanAinda não há avaliações
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Documento19 páginasEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uAinda não há avaliações