Escolar Documentos
Profissional Documentos
Cultura Documentos
RM
Enviado por
Thitamhrn0 notas0% acharam este documento útil (0 voto)
7 visualizações25 páginas,..
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documento,..
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
7 visualizações25 páginasRM
Enviado por
Thitamhrn,..
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 25
Terminology and Classification
Four types of hypertensive disease:
•Gestational hypertension—evidence for the
preeclampsia syndrome does not develop and
hypertension resolves by 12 weeks postpartum
•Preeclampsia and eclampsia syndrome
•Chronic hypertension of any etiology
•Preeclampsia superimposed on chronic
hypertension.
Diagnosis
• Hypertension is diagnosed empirically when
appropriately taken blood pressure exceeds
140 mm Hg systolic or 90 mm Hg diastolic.
Gestational Hypertension
• Diagnosis is made in women whose blood
pressures reach 140/90 mm Hg or greater for
the first time after midpregnancy, but in
whom proteinuria is not identified.
• Gestational hypertension is reclassifed as
transient hypertesion if evidence for
preeclampsia does not develop and the blood
pressure returns to normal by 12 weeks
postpartum.
Preeclampsia Syndrome
• Preeclampsia is best described as a
pregnancy-specific syndrome that can affect
virtually every organ system.
• Appearance of proteinuria remains an
important diagnosis criterion.
• Proteinuria is an objective marker and reflects
the system-wide endothelial leak, which
characterizes the preeclampsia syndrome.
Eclampsia
• In a woman with preeclampsia, a convulsion
that cannot be attributed to another cause is
termed eclampsia.
• May appear before, during, or after labor.
Preeclampsia Superimposed on
Chronic Hypertension
• Chronic hypertensive disorder predisposes a woman to
develop superimposed preeclampsia syndrome
• Blood pressures ≥ 140/90 mm Hg before pregnancy or
before 20 weeks’ gestation, or both.
• In some women with chronic hypertension, their blood
pressure increases to obviously abnormal levels, and this is
typically after 24 weeks.
• If new-onset or worsening baseline hypertension is
accompanied by new-onset proteinuria or other findings,
then superimposed preeclampsia is diagnosed.
• Compared with “pure” preeclampsia, superimposed
preeclampsia commonly develops earlier in pregnancy. It
also tends to be more severe and often is accompanied by
fetal-growth restriction.
Etiology
Those currently considered important include:
• Placental implantation with abnormal
trophoblastic invasion of uterine vessels
• Immunological maladaptive tolerance between
maternal, paternal (placental), and fetal tissues
• Maternal maladaptation to cardiovascular or
inflammatory changes of normal pregnancy
• Genetic factors including inherited predisposing
genes and epigenetic influences.
Abnormal Trophoblastic Invasion
Immunological Factors
• Loss of maternal immune tolerance to paternally
derived placental and fetal antigens
• The histological changes at the maternal-placental
interface are suggestive of acute graft rejection.
• Some of the factors possibly associated with
dysregulation include “immunization” from a previous
pregnancy, some inherited human leukocyte antigen
(HLA) and natural killer (NK)-cell receptor haplotypes,
and possibly shared susceptibility genes with diabetes
and hypertension
Nutritional Factors
• A diet high in fruits and vegetables with
antioxidant activity is associated with
decreased blood pressure.
• Incidence of preeclampsia was doubled in
women whose daily intake of ascorbic acid
was less than 85 mg
Genetic Factors
• Incident risk for preeclampsia of 20 to 40
percent for daughters of preeclamptic
mothers;
• 11 to 37 percent for sisters of preeclamptic
women;
• 22 to 47 percent for twins.
Management
Basic management objectives for any pregnancy
complicated by preeclampsia are:
• termination of pregnancy with the least possible
trauma to mother and fetus
• birth of an infant who subsequently thrives
• complete restoration of health to the mother.
In many women with preeclampsia, especially those
at or near term, all three objectives are served
equally well by induction of labor. One of the most
important clinical questions for successful
management is precise knowledge of fetal age.
Management
• Termination of pregnancy is the only cure for
preeclampsia.
• When the fetus is preterm, the tendency is to
temporize in the hope that a few more weeks in
utero will reduce the risk of neonatal death or
serious morbidity from prematurity.
• With moderate or severe preeclampsia that does
not improve after hospitalization, delivery is
usually advisable for the welfare of both mother
and fetus.
Management for suspected severe
preeclampsia
Early Diagnosis of Preeclampsia
• Women with new-onset diastolic blood pressures > 80
mm Hg but < 90 mm Hg or with sudden abnormal
weight gain of more than 2 pounds per week includes,
at minimum, return visits at 7-day intervals.
• Outpatient surveillance is continued unless overt
hypertension, proteinuria, headache, visual
disturbances, or epigastric discomfort supervene.
• Women with overt new-onset hypertension— either
diastolic pressures ≥ 90 mm Hg or systolic pressures ≥
140 mm Hg—are admitted to determine if the increase
is due to preeclampsia, and if so, to evaluate its
severity.
Evaluation
A systematic evaluation is instituted to include the following:
• Detailed examination, which is followed by daily scrutiny
for clinical findings such as headache, visual disturbances,
epigastric pain, and rapid weight gain
• Weight determined daily
• Analysis for proteinuria or urine protein:creatinine ratio on
admittance and at least every 2 days thereafter
• Blood pressure readings in the sitting position with an
appropriate-size cuff every 4 hours, except between 2400
and 0600 (unless previous readings had become elevated )
• Measurements of plasma or serum creatinine and hepatic
aminotransferase levels and a hemogram that includes
platelet quantification
• Evaluation of fetal size and well-being and amnionic fluid
volume, with either physical examination or sonography.
Eclampsia Management
• Control of convulsions using an intravenously administered
loading dose of magnesium sulfate that is followed by a
maintenance dose, usually intravenous, of magnesium
sulfate
• Intermittent administration of an antihypertensive medica-
tion to lower blood pressure whenever it is considered
dangerously high
• Avoidance of diuretics unless there is obvious pulmonary
edema, limitation of intravenous uid administration unless
uid loss is excessive, and avoidance of hyperosmotic agents
• Delivery of the fetus to achieve a remission of
preeclampsia.
Management of Severe Hypertension
Hydralazine
• administered intravenously with a 5-mg initial
dose, and this is followed by 5- to 10-mg doses at
15- to 20-minute intervals until a satisfactory
response is achieved
• target response antepartum or intrapartum is a
decrease in diastolic blood pressure to 90 to 110
mm Hg
• target response antepartum or intrapartum is a
decrease in diastolic blood pressure to 90 to 110
mm Hg
Labetalol
•target response antepartum or intrapartum is a
decrease in diastolic blood pressure to 90 to 110
mm Hg
•10 mg intravenously initially
•If the blood pressure has not decreased to the
desirable level in 10 minutes, then 20 mg is given.
The next 10-minute incremental dose is 40 mg and
is followed by another 40 mg if needed. If a salutary
response is not achieved, then an 80-mg dose is
given. (max dose 220mg)
Hydralazine versus Labetalol
• Hydralazine caused significantly more
maternal tachycardia and palpitations,
whereas labetalol more frequently caused
maternal hypotension and bradycardia.
• Both drugs have been associated with a
reduced frequency of fetal heart rate
accelerations
Nifedipin
• Randomized trials that compared nifedipine
with labetalol found neither drug de nitively
superior to the other. However, Nifedipin
lowered blood pressure more quickly
• Recommend a 10-mg initial oral dose to be
repeated in 30 minutes if necessary
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Hoarseness and Laryngopharyngeal RefluxDocumento5 páginasHoarseness and Laryngopharyngeal RefluxThitamhrnAinda não há avaliações
- HypertensionDocumento52 páginasHypertensionpatriciajesikaAinda não há avaliações
- Pemicu 1 Endokrin MargaretDocumento60 páginasPemicu 1 Endokrin MargaretThitamhrnAinda não há avaliações
- Recap MR02-041118A: AlbertDocumento5 páginasRecap MR02-041118A: AlbertThitamhrnAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Health History QuestionnaireDocumento3 páginasHealth History QuestionnairejlaferriereAinda não há avaliações
- Traditional indian medicine.அகஸ்தியர் சித்த வைத்திய நிலையம் - AGASTHIAR ALL DIESEACESDocumento26 páginasTraditional indian medicine.அகஸ்தியர் சித்த வைத்திய நிலையம் - AGASTHIAR ALL DIESEACESDeebaAinda não há avaliações
- AMC Clinical Recalls 2019 (COMPLETE TILL JUL) - SponsoredDocumento46 páginasAMC Clinical Recalls 2019 (COMPLETE TILL JUL) - SponsoredIgor Dias67% (3)
- Introduction To Oral Pathology 1Documento32 páginasIntroduction To Oral Pathology 1Hoor M TahanAinda não há avaliações
- DM, DKA, and IDMDocumento19 páginasDM, DKA, and IDMJennyu YuAinda não há avaliações
- Vol 27.5 - Neurocritical Care.2021Documento363 páginasVol 27.5 - Neurocritical Care.2021RafaelAinda não há avaliações
- Hema 1 ErythropoiesisDocumento20 páginasHema 1 Erythropoiesismarie judimor gomezAinda não há avaliações
- Peds Ati ReviewDocumento32 páginasPeds Ati ReviewMorgan100% (41)
- English Robot Script FinalDocumento4 páginasEnglish Robot Script FinalKumaresh MuthuAinda não há avaliações
- High-Risk Newborns and Child During Illness and Hospitalization - Pediatric NursingDocumento200 páginasHigh-Risk Newborns and Child During Illness and Hospitalization - Pediatric Nursingjaggermeister20100% (8)
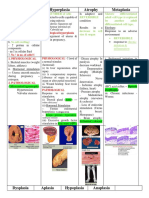
- Hypertrophy Hyperplasia Atrophy MetaplasiaDocumento20 páginasHypertrophy Hyperplasia Atrophy MetaplasiaYunQingTanAinda não há avaliações
- Muscle Weakness in Adults PDFDocumento14 páginasMuscle Weakness in Adults PDFJames TianAinda não há avaliações
- Cardiac Function Tests Anatomy of The HeartDocumento8 páginasCardiac Function Tests Anatomy of The HeartJosiah BimabamAinda não há avaliações
- Infecciones Necrotizantes de Tejidos Blandos TheLancet 2023Documento14 páginasInfecciones Necrotizantes de Tejidos Blandos TheLancet 2023Nicolás LaverdeAinda não há avaliações
- 2012 Mrcog 1 RecallsDocumento17 páginas2012 Mrcog 1 RecallsMahavir GemavatAinda não há avaliações
- Icd 10 CodeDocumento3 páginasIcd 10 Codecheryll duenasAinda não há avaliações
- Lichen Striatus Successfully Treated With Photodynamic TherapyDocumento3 páginasLichen Striatus Successfully Treated With Photodynamic TherapyOzheanAMAinda não há avaliações
- Common Symptoms of Gastrointestinal and Abdominal DiseaseDocumento34 páginasCommon Symptoms of Gastrointestinal and Abdominal DiseaseMalueth AnguiAinda não há avaliações
- Neuro UrologyDocumento53 páginasNeuro UrologymoominjunaidAinda não há avaliações
- Case Study GonorrheaDocumento19 páginasCase Study GonorrheaErika ThereseAinda não há avaliações
- 93 - 08 Bantar 7 Hal 306-312Documento7 páginas93 - 08 Bantar 7 Hal 306-312amilyapraditaAinda não há avaliações
- Systemic Inflammatory Response Syndrome The CurrenDocumento6 páginasSystemic Inflammatory Response Syndrome The CurrenberlianAinda não há avaliações
- Adult Referral For PC Assessment FormDocumento1 páginaAdult Referral For PC Assessment Formwhy u reading thisAinda não há avaliações
- Clinico-Radiological Profile in Covid - 19 PatientsDocumento6 páginasClinico-Radiological Profile in Covid - 19 PatientsInternational Journal of Innovative Science and Research Technology100% (1)
- Start CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorDocumento2 páginasStart CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorFelicia ErikaAinda não há avaliações
- Dental Pulse 12th Ed - PhysiologyDocumento107 páginasDental Pulse 12th Ed - PhysiologyLangAinda não há avaliações
- Rife FrequenciesDocumento471 páginasRife Frequencieslopans100% (9)
- Moving Exam NCM 109 Lecture For PrintDocumento6 páginasMoving Exam NCM 109 Lecture For PrintMoneto CasaganAinda não há avaliações
- Cerebral Salt Wasting Syndrome - StatPearls - NCBI BookshelfDocumento4 páginasCerebral Salt Wasting Syndrome - StatPearls - NCBI BookshelfOnggo WiliyantoAinda não há avaliações
- Sistema Curativo Por Dieta Amucosa - Arnold Ehret - WWW - Arnoldehret.infoDocumento8 páginasSistema Curativo Por Dieta Amucosa - Arnold Ehret - WWW - Arnoldehret.infoLorena CalahorroAinda não há avaliações