Escolar Documentos
Profissional Documentos
Cultura Documentos
Course 2: Origin, Destination and Structure of Cells and Tissues of The Immune System
Enviado por
CristinaGheorghe0 notas0% acharam este documento útil (0 voto)
32 visualizações29 páginas---
Título original
Immunology
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PPTX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documento---
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
32 visualizações29 páginasCourse 2: Origin, Destination and Structure of Cells and Tissues of The Immune System
Enviado por
CristinaGheorghe---
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PPTX, PDF, TXT ou leia online no Scribd
Você está na página 1de 29
Course 2: Origin, destination and structure of
cells and tissues of the immune system
• Bone Marrow
• Stem Cells
• Erythropoiesis
• Granulolcytopoiesis
• Eosinophils
• Basophils
• Neutrophls
• Lymphopoiesis
• Natural Killer Cells
• Monocytes
• Dendritic Cells
• Thymus
• Lymph Nodes
• Spleen
• Mucosal Associated Lymphoid Tissue (MALT)
• Circulation and Recirculation
Course 2: Immunology, Prof. Ileana Constantinescu 1
BONE MARROW
• The bone marrow constitutes almost 5% of
total body weight and is responsible for the
formation of all blood (hemopoiesis) in
adults.
• It also provides a microenvironment necessary
for B lymphocyte maturation and formation of
pre-T cells (lymphopoiesis).
Course 2: Immunology, Prof. Ileana Constantinescu 2
STEM CELLS
• All of these cells originate from undifferentiated
pluripotential hemopoietic stem cells (PHSC), which
can be found first in the mammalian embryo within the
liver then spleen.
• SCs are pluripotential CD34+ and represent less than
0.1 % of all cells in adult marrow. SCs have limited
proliferative capacity and exhibit the potential to
differentiate into all cells of the myeloid (erythrocytes,
granulocytes, monocytes, and platelets) or lymphoid (T
and B cells) lineage. When SCs divide, the two
daughter cells (DCs) can either continue as SCs or
proceed into any of the differentiation pathways
Course 2: Immunology, Prof. Ileana Constantinescu 3
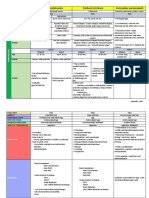
Cells of the immune system - hematopoiesis
Course 2: Immunology, Prof. Ileana Constantinescu 4
Cells and growth factors in hemopoiesis
Course 2: Immunology, Prof. Ileana Constantinescu 5
• If a DC (daughter cell) proceeds into the differentiation pathway,
it becomes a dividing multipotential colony forming unit-spleen
(CFU-S) or CFU (colony forming unit-lymphoid )(CFU-Ly)
progenitor cell and then a progressively maturing unipotential
precursor cell for any of the mature cells of peripheral blood. The
precursor cell gradually loses its ability to self-renew and then
divide as it approaches its mature phenotype.
• SCs not only depend on a specific microenvironment for their
maturation, they also depend on numerous glycoprotein growth
factors that act at different stages to control the cell type as well
as rate of cell formation. Some of these growth factors such as
stem cell factor (SCF) and interleukin (IL-7) are secreted by
marrow stromal cells, but most others are produced elsewhere
and transported to the marrow by the blood stream (endocrine).
Course 2: Immunology, Prof. Ileana Constantinescu 6
ERYTHROPOIESIS
• Erythropoiesis occurs when a CFU-S cell gives rise to burst-forming
units - erythrocyte (BFU-E) and then colony-forming units-
erythrocyte (CFU-E) all under the influence of erythropoietin (EPO)
from the kidney cortex as well as IL-3 and granulocyte-macrophage
colony-stimulating factor (GM-CSF).
• CFU-E form the precursor of erythrocytes, the proerythroblast. Under
normal conditions, 2.5 X 10 11 erythrocytes are produced each day.
Proerythroblast —► basophilic erythroblast —►
polychromatophilic erythroblast —> ortho-chromatophilic
erythroblast —» reticulocyte —» erythrocyte is the sequence of
events in maturation. During this sequence, the nucleus is condensed
and then lost as the cell becomes 6-7 micro.
• These maturation events occur around macrophages, which
phagocytose the extruded nuclei as well as provide some growth
factors.
Course 2: Immunology, Prof. Ileana Constantinescu 7
GRANULOCYTOPOIESIS
• Granulocytopoiesis is the generation of three
types of granulocytes (neutrophils,
eosinophils, basophils) from CFU-S.
• Mature cells are named because of staining of
their specific granules. All derive from CFU-S
(spleen) —> CFU-Eo, -BASO or CFU-NM -+
CFU-N -* myeloblast -* promyelocyte —>
myelocyte -* metamyelocyte -H» Stab -*
mature cell.
Course 2: Immunology, Prof. Ileana Constantinescu 8
Eosinophils
• Eosinophils require GM-CSF, IL-3, and IL-5 for
their maturation. They represent 2 to 4% of
peripheral blood white cells. Their specific
granules contain a number of factors including
histaminase, acid phosphatase, and major
basic protein. They are important in
destroying parasites, phagocytosing antigen-
antibody complexes, and combating
histamine levels during allergic reactions.
Course 2: Immunology, Prof. Ileana Constantinescu 9
Basophils
• Basophils require GM-CSF. IL-3, and IL-4 for
their maturation. They represent <1% of
peripheral blood white cells. Their specific
granules contain histamine, heparin, and
chemotactic factors for eosinophils and
neutrophils.
• They are similar to mast cells in that they
participate in IgE-mediated immediate
hypersensitivity responses.
Course 2: Immunology, Prof. Ileana Constantinescu 10
Neutrophils
• Neutrophils require GM-CSF, IL-3, and granulocyte
colony-stimulating factor (G-CSF) for their maturation.
Unlike eosinophils and basophils, the CFU-S gives rise
to a CFU-NM cell, which, depending on the level of
granulocyte or macrophage colony-stimulating factor in
the environment, can differentiate into a CFU-Neut or
CFU-M cell. 60% to 70% of all white cells are
neutrophils.
• Their specific granules contain alkaline phosphatase,
lysozyme, lactoferrin, phagocytic and type IV
collagenase. They are the earliest phagocytic cells to
appear in a bacterial infection and are a prominent
constituent of cellular immune response.
Course 2: Immunology, Prof. Ileana Constantinescu 11
LYMPHOPOIESIS
• Lymphopoiesis is the ability of CFU-Ly to form either
CFU-LyB or CFU-LyT in the bone marrow.
• CFU-LyB cells develop in the presence of IL-7 and IL-3 in
the marrow to immunocompetent B cells with slgM.
• Further maturation of these cells occurs in germinal
centers of secondary lymphoid tissue. CFU-Ly T cells
become pre-T cells, which leave the bone marrow and
find their way to the subcapsular area of the thymic
cortex where they proliferate and mature in the deeper
thymic cortex into either CD3 + 4+ or CD3 + 8+ cells.
• Thus, the bone marrow and thymus are considered
primary lymphoid tissue, and lymph nodes, spleen,
gut-associated lymphoid tissue, etc. are considered
secondary lymphoid tissue.
Course 2: Immunology, Prof. Ileana Constantinescu 12
NATURAL KILLER CELLS
• Natural killer (NK) cells also develop within the
marrow and then are found in peripheral
blood, liver sinusoids (pit cells), and spleen
sinusoids but not thoracic lymph. duct.
• NK cells appear early in bacterial infections,
can secrete interferon-y, and spontaneously
kill some viral infected cells and tumor cells.
• They respond to IL-2 and develop
independently of the thymus.
Course 2: Immunology, Prof. Ileana Constantinescu 13
MONOCYTES
• Monocytes develop from CFU-M progenitors under the influence of GM-
CSF, IL-3, and G-CSF. They represent 3 to 8% of leukocytes in peripheral
blood.
• Monocytes have numerous azurophilic granules (lysosomes) in their
cytoplasm and can readily leave the circulation to give rise to
macrophages within almost every organ. They are thus the source of the
mononuclear phagocytic system throughout the body.
• They are even more phagocytic than neutrophils or eosinophils in that
they can degrade larger bacteria within phagosomes via the formation of
hydrogen peroxide, hypochlorous acid, and superoxide.
• They can also fuse to form foreign body giant cells in response to a large
antigenic load. Macrophages express class II major histocompatibility
complex and can function as antigen-processing and -presenting cells.
They secrete the pro-inflammatory cytokines IL-1, IL-6, and tumor necrosis
factor a (TNFα) upon activation.
Course 2: Immunology, Prof. Ileana Constantinescu 14
DENDRITIC CELLS
• Dendritic cells are bone marrow-derived cells
specialized for presenting antigens to either CD4 +
or CD8+ T cells in order to initiate a primary
immune response.
• These cells appear to be generated from CD34+
cells and require GM-CSF, TNF alpha, and
possibily TGF beta for full maturation. Dendritic
cells are found in all lymphoid tissues where they
have specific names. Because of their highly
efficient function in antigen presentation, they
have come to be called "nature's adjuvant“.
Course 2: Immunology, Prof. Ileana Constantinescu 15
Course 2: Immunology, Prof. Ileana Constantinescu 16
THYMUS
• The thymus is a primary lymphoid organ that is required
for the generation of immunocompetent CD3+4+ and CD3 +
8+ cells necessary for an adaptive immune response .
• The stroma of the thymus is composed of epithelial cells
that originate from the third pharyngeal pouch in the
embryo. The parenchyma is made up of thymocytes that
are either positively and then negatively selected for
maturation (<1%) or deleted (>99%) by apoptosis.
• Most of the deletion of cells occurs in the cortex, with the
medulla containing mainly mature cells.
• After slg+ B cells, pre-T cells, monocytes, NK cells, and
dendritic cells have developed in the marrow and CD3+4+
and CD3+ 8+ cells have matured in the thymus, they leave
these primary lymphoid organs and migrate into peripheral
secondary lymphoid tissue: lymph nodes spleen and
mucosal associated lymphoid tissue (MALT).
Course 2: Immunology, Prof. Ileana Constantinescu 17
LYMPH NODES
• Lymph nodes (LNs) are encapsulated structures
that are strategically placed throughout the body
to receive and filter antigens and cells from
peripheral interstitial fluid and lymph.
• All LNs eventually drain into the thoracic duct
system and back to the peripheral blood.
• There are approximately 550 kidney-shaped, 1-10
mm in diameter, lymph nodes in the body. Their
indented hilus contains blood and lymphatic
vessels.
Course 2: Immunology, Prof. Ileana Constantinescu 18
Structure of a lymph node
Course 2: Immunology, Prof. Ileana Constantinescu 19
• Thus, LNs have two circulations, lymph and blood,
which permeate a stroma of largely type III and I
collagen. The type III collagen is arranged in a chicken
wire fashion, forming lymphatic sinuses supporting a
parenchyma of immunocompetent T and B cells as well
as macrophages and other antigen-presenting cells.
These cells are localized into:
• SUPERFICIAL CORTEX: containing primary and
secondary follicles with germinal centers containing
dark and light zones;
• DEEP CORTEX: containing high endothelial post-
capillary venules;
• MEDULLA: with medullary cords.
Course 2: Immunology, Prof. Ileana Constantinescu 20
• Lymph enters a Lymph nod (LN) at its surface as numerous afferent
lymphatics pierce its type I collagenous capsule and empty into the
subcapsular sinus. It then percolates through the cortex into the
medullary sinuses, where it leaves the hilus via efferent lymphatics.
Any cells that enter through afferent lymphatics can also enter the
parenchyma of the LN.
• The hilar artery supplies the medulla and deep cortex but then
empties into a capillary net on either side of the superficial cortical
follicles. These capillaries then drain into post capillary venules
(PCVs) with a very high cuboidal endothelium in the deep cortex.
They then decrease their endothelial height, pass through the
medulla, and leave the LN as hilar veins. It is at the PCVs (post
capillary senules) in the deep cortex where circulating T and B cells
adhere to PCV endothelium and migrate between these cells
(diapedesis) into the node.
• Most B cells migrate superficially into follicles, with most of the T
cells remaining in the deep cortex. They can remain in the LN for an
undetermined period or enter a lymph sinus and exit via an efferent
lymphatic. We will develop further the structure of the LN during an
immune response.
Course 2: Immunology, Prof. Ileana Constantinescu 21
SPLEEN
• The spleen is an encapsulated organ with
lymphoid tissue called white pulp (WP), which
can respond to blood-borne antigens surrounded
by red pulp (RP). More lymphocytes circulate
through it each day than any other secondary
lymphoid organ.
• Similar to LN, the spleen has a stroma of type III
and I (capsule and trabecular) collagen that
supports the parenchyma of WP and a blood
sinusoidal system with cords of hemopoietic and
lymphoid tissue called RP separated from each
other by a marginal zone.
Course 2: Immunology, Prof. Ileana Constantinescu 22
Structure of spleen white pulp with periarteriolar lymphoid sheath (PALS)
Course 2: Immunology, Prof. Ileana Constantinescu 23
Course 2: Immunology, Prof. Ileana Constantinescu 24
• The part of the WP around a central arteriole is called the
periarteriolar lymphoid sheath (PALS) and contains primarily T
cells. It is thus analogous to the deep cortex of LN. The periphery of
WP contains B cellrich lymphoid follicles just like the periphery of
LN. Between the periphery of the WP and the marginal zone is a
blood filled marginal sinus, which receives capillary branches from
the central arteriole. T and B cells leave the splenic circulation here
and then migrate to the PALS or follicles, respectively.
• The marginal zone contains macrophages and some memory B
cells. The marginal zone and sinus function as a part of B and T cell
entry points into the WP similar to high endothelial venules of LN,
but the marginal sinus has a low endothelium. B and T cells can
migrate out of the WP into an RP cord through bridging channels
(BCs) in the marginal zone.
• The RP contains blood sinusoids with associated macrophages that
line cellular cords. Some RP cords contain granulocytes, but others
connect with WP follicles and contain plasma cells. The sinusoidal
macrophages destroy old platelets and erythrocytes. The central
arterioles empty directly into the RP cord or sinuses and then into
trabecular veins.
Course 2: Immunology, Prof. Ileana Constantinescu 25
MUCOSAL ASSOCIATED LYMPHOID TISSUE (MALT)
• The epithelial lining, lamina propria, and submucosa of the
gastrointestinal, respiratory, and genitourinary tracts contain
wandering cells, diffuse aggregates, solitary primary nodules, or
aggregates of secondary nodules that can become encapsulated. All
of these are collectively called mucosal associated lymphoid tissue
(MALT).
• While most of the diffuse and aggregated lymphoid tissue of the
MALT is responsible for producing IgA, most intraepithelial
lymphocytes (IEL) are CD8+ αβ (60%) or γδ(40%) T cells. It appears
that the γδ cells may react to bacterial antigens. The epithelial
lining over Peyer's patches (PP) contains specialized antigen
transporting cells called M cells, which transport luminal antigen to
under lying antigen reactive lymphocytes.
• It should also be realized that most of the cells activated in the
MALT stay in or return to the MALT. Thus, cells stimulated in PP
(Peyper’s patches) or tonsils enter mesenteric or cervical lymph
nodes for further maturation. After re-entering the circulation, they
home back to the MALT.
Course 2: Immunology, Prof. Ileana Constantinescu 26
Course 2: Immunology, Prof. Ileana Constantinescu 27
CIRCULATION AND RECIRCULATION
Both T and B cells continuously circulate and recirculate, blood —> lymph —>
blood. Approximately 1-2% recirculate every hour. However, NK cells are only
found in blood, spleen, and liver.
Course 2: Immunology, Prof. Ileana Constantinescu 28
Questions
1. Which are the primary and the secondary lymphoid organs?
2. Which is the main role of bone marrow?
3. Which are the main characteristics of stem cells?
4. Which are the stages of erythropoiesis?
5. Which are the stages granulocitopoiezei?
6. Which are the stages limfopoiezei?
7. Which are the main types of granulocytes and their role in the immune
response?
8. How does the NK cells?
9. Antigen presenting cells: examples, their role in the immune response
10. What is the role of the thymus?
11. Briefly describe lymph node structure
12. What is mucosal-associated lymphoid tissue and the role in the immune
defense?
13. What means the circulation and recirculation of the lymphocytes?
Você também pode gostar
- Vital Spots 10 - Taranaki ITF Taekwondo PDFDocumento54 páginasVital Spots 10 - Taranaki ITF Taekwondo PDFMaria Elisa MonclusAinda não há avaliações
- Phoneme Flip Chart-2Documento4 páginasPhoneme Flip Chart-2api-217065852100% (1)
- MHC I Proteins, Which Present Antigens To Cytotoxic T Cells, (2) MHC II Proteins, Which Present Antigens T Helper CellsDocumento25 páginasMHC I Proteins, Which Present Antigens To Cytotoxic T Cells, (2) MHC II Proteins, Which Present Antigens T Helper CellsMudassar Roomi100% (1)
- Types of EnemaDocumento6 páginasTypes of EnemaOmprakash Saini100% (2)
- Thalassemi ADocumento23 páginasThalassemi Ainterna MANADO100% (1)
- Blood Cells, Immunity and Blood ClottingDocumento65 páginasBlood Cells, Immunity and Blood Clottingmunaamuummee100% (1)
- Cell Cycle: - Dr. Ishita SinghalDocumento69 páginasCell Cycle: - Dr. Ishita SinghalDR. ISHITA SINGHAL100% (1)
- LIVERDocumento18 páginasLIVERShivaniLeela100% (3)
- Use action buttons to navigate tutorialDocumento49 páginasUse action buttons to navigate tutorialleeAinda não há avaliações
- Cytokines, Immunological Memory and Types of Adaptive ImmunityDocumento10 páginasCytokines, Immunological Memory and Types of Adaptive ImmunitySamah AbboAinda não há avaliações
- Antigens - Definition, Properties, Types & Antigen RecognitionDocumento11 páginasAntigens - Definition, Properties, Types & Antigen RecognitionАнна КатраженкоAinda não há avaliações
- Leucocytes 160619161725Documento44 páginasLeucocytes 160619161725Rohit K Y100% (1)
- Membrane Transport Mechanisms and HomeostasisDocumento29 páginasMembrane Transport Mechanisms and Homeostasisramadan100% (1)
- Humoral & Celullar ImmunityDocumento60 páginasHumoral & Celullar ImmunityHaziq KamardinAinda não há avaliações
- Autoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistDocumento52 páginasAutoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistZubair YousafAinda não há avaliações
- Immunogens Or Antigens: Key Differences ExplainedDocumento51 páginasImmunogens Or Antigens: Key Differences ExplainedSteph VeeAinda não há avaliações
- Pharmacodynamics3 161031154812Documento43 páginasPharmacodynamics3 161031154812Adeel Khan100% (1)
- Vector - and Rodent-Borne Diseases in Europe and North America 2gfshDocumento411 páginasVector - and Rodent-Borne Diseases in Europe and North America 2gfshRhyan ArfanAinda não há avaliações
- Basic Immunology ExplainedDocumento41 páginasBasic Immunology ExplainedFebri Yudha Adhi Kurniawan100% (1)
- Degeneration & Regeneration of Nerve FibreDocumento29 páginasDegeneration & Regeneration of Nerve FibreSana FatimaAinda não há avaliações
- 2021 Host Reponse To InfectionDocumento38 páginas2021 Host Reponse To Infectionmaggie100% (1)
- The Fate of Metabolism Andmabolic PathwaysDocumento25 páginasThe Fate of Metabolism Andmabolic PathwaysXuân Vi100% (1)
- Innate & Adaptive Immunity (DR - Soraya Rezeki, MKT)Documento30 páginasInnate & Adaptive Immunity (DR - Soraya Rezeki, MKT)Dyah Wahlia100% (1)
- 5 HypoxiaDocumento42 páginas5 HypoxiaShanzayAinda não há avaliações
- Physiology ManualDocumento80 páginasPhysiology ManualNoreen Orro Bernal100% (2)
- Acute Febrile IllnessDocumento23 páginasAcute Febrile IllnessSalih Anwar50% (2)
- The Immune System ExplainedDocumento82 páginasThe Immune System ExplainedMa Divina Kristi DiscarAinda não há avaliações
- Bone TissueDocumento66 páginasBone TissueFunikawati Baldiyah100% (1)
- Cells and Organs of The Immune System 2015 SV (1Documento77 páginasCells and Organs of The Immune System 2015 SV (1Muneeb ArshadAinda não há avaliações
- Introduction To Physiology: General Physiology The Cell HomeostasisDocumento38 páginasIntroduction To Physiology: General Physiology The Cell HomeostasisAnanta Subedi100% (1)
- Plant Innate Immunity: Sub. - Biochem-506, IMMUNO CHEMISTRYDocumento22 páginasPlant Innate Immunity: Sub. - Biochem-506, IMMUNO CHEMISTRYviralnanobio_4150420Ainda não há avaliações
- Apoptosis and CancerDocumento20 páginasApoptosis and CancerSajjad Ahmad0% (1)
- Innate and Adaptive Immunity: Cells, Organs and FunctionsDocumento17 páginasInnate and Adaptive Immunity: Cells, Organs and FunctionsBasma RagabAinda não há avaliações
- ICD 10 Codes for Tuberculosis (TB) DiseasesDocumento111 páginasICD 10 Codes for Tuberculosis (TB) DiseasesMarnitaAinda não há avaliações
- Cellular ImmunityDocumento13 páginasCellular ImmunityPragya100% (1)
- Apoptosis by Dr. Sanjiv Kumar-1Documento27 páginasApoptosis by Dr. Sanjiv Kumar-1चौधरी हरिओम सौरोतAinda não há avaliações
- Organs of The Immune SystemDocumento19 páginasOrgans of The Immune SystemprabuAinda não há avaliações
- Differential White Blood Cell CountDocumento20 páginasDifferential White Blood Cell CountNada hasan100% (2)
- Immune Response DRPath Part 1Documento71 páginasImmune Response DRPath Part 1SITI NUR FA'IZULBA'EDAH BINTI MAT RAZIAinda não há avaliações
- Enzymology: Discuss About Regulation of Enzyme ActivityDocumento4 páginasEnzymology: Discuss About Regulation of Enzyme ActivityNorrifhan Akmal IsmailAinda não há avaliações
- Neutrophils: in Health and DiseaseDocumento65 páginasNeutrophils: in Health and DiseaseKush Pathak100% (1)
- Bio 132 Chapter 18 NotesDocumento8 páginasBio 132 Chapter 18 Noteslovelyc95100% (1)
- Physiology L6Documento6 páginasPhysiology L6Anonymous elq7jZiSAinda não há avaliações
- Cell Communication PDFDocumento109 páginasCell Communication PDFediaz_956003100% (1)
- Nerve Muscle PhysioDocumento30 páginasNerve Muscle Physiopatel_hanisha06Ainda não há avaliações
- Hexose Monophosphate Shunt Pathway Generates NADPH and Ribose-5-PhosphateDocumento7 páginasHexose Monophosphate Shunt Pathway Generates NADPH and Ribose-5-PhosphateElla BangalanAinda não há avaliações
- Signal TransductionDocumento38 páginasSignal Transductionjuju100% (2)
- Anterior Pituitary HormonesDocumento46 páginasAnterior Pituitary Hormonespramod bhaleraoAinda não há avaliações
- Haemotology Notes Haemotology Notes: Medicine (University of Glasgow) Medicine (University of Glasgow)Documento20 páginasHaemotology Notes Haemotology Notes: Medicine (University of Glasgow) Medicine (University of Glasgow)shravaniAinda não há avaliações
- Small IntestineDocumento16 páginasSmall IntestineShimmering MoonAinda não há avaliações
- Endo 3 Notes PDFDocumento9 páginasEndo 3 Notes PDFDilAinda não há avaliações
- HomeostasisDocumento25 páginasHomeostasisCooper Puno100% (1)
- Thyroid and Parathyroid GlandsDocumento23 páginasThyroid and Parathyroid Glandsmoimoi819Ainda não há avaliações
- Antibodies Structure and FunctionDocumento16 páginasAntibodies Structure and Functionياسين احمد علي الشيخAinda não há avaliações
- Gell & Coomb's Classification of Hypersensitivity ReactionsDocumento10 páginasGell & Coomb's Classification of Hypersensitivity ReactionsRashed ShatnawiAinda não há avaliações
- Basic Immunology: An Overview of the Immune System and Its FunctionsDocumento101 páginasBasic Immunology: An Overview of the Immune System and Its FunctionsZas VutraAinda não há avaliações
- Presented By: DR Sharmila G SDocumento76 páginasPresented By: DR Sharmila G SSharmila Shivakumar G SAinda não há avaliações
- Apoptosis tutorial notes: Understanding programmed cell deathDocumento8 páginasApoptosis tutorial notes: Understanding programmed cell deathismealAinda não há avaliações
- CH 11 PPT Cell Communication 1Documento77 páginasCH 11 PPT Cell Communication 1api-270681964Ainda não há avaliações
- Embryo NotesDocumento52 páginasEmbryo NotesSharona Avgush100% (1)
- Topic: Cytokine and Their Roles in The Immune Regulation: Md. Jiyaul MustafaDocumento21 páginasTopic: Cytokine and Their Roles in The Immune Regulation: Md. Jiyaul MustafaAisha Siddiq100% (1)
- Neuronal CommunicationDocumento29 páginasNeuronal CommunicationSamantha CAinda não há avaliações
- SGD Physiology Endocrine and MetabolismDocumento7 páginasSGD Physiology Endocrine and MetabolismTinesh RajahAinda não há avaliações
- 3rd Lecture On Skeletal Muscle Physiology by DR - RoomiDocumento21 páginas3rd Lecture On Skeletal Muscle Physiology by DR - RoomiMudassar Roomi67% (3)
- 04 AntigenDocumento30 páginas04 AntigenVivin Syamsul ArifinAinda não há avaliações
- Ligand Cell Signaling PathwaysDocumento117 páginasLigand Cell Signaling PathwaysShoaib MomenAinda não há avaliações
- Lecture 1 - Introduction To HematologyDocumento30 páginasLecture 1 - Introduction To Hematologyimam100% (1)
- Two-Dimensional Gel Electrophoresis of Proteins: Methods and ApplicationsNo EverandTwo-Dimensional Gel Electrophoresis of Proteins: Methods and ApplicationsJulio CelisAinda não há avaliações
- Congenital Heart DiseaseDocumento83 páginasCongenital Heart DiseaseArleen MatincaAinda não há avaliações
- Cystic fibrosis – an overviewDocumento60 páginasCystic fibrosis – an overviewArleen MatincaAinda não há avaliações
- Growth and Development: A Multifactorial ProcessDocumento41 páginasGrowth and Development: A Multifactorial ProcessCristinaGheorgheAinda não há avaliações
- Ckd. CKF 2020Documento20 páginasCkd. CKF 2020CristinaGheorgheAinda não há avaliações
- Immunodeficiencies - Dr. BergheaDocumento50 páginasImmunodeficiencies - Dr. BergheaCristinaGheorgheAinda não há avaliações
- Toxicology Symptoms and Coma SignsDocumento52 páginasToxicology Symptoms and Coma SignsMunteanu LauraAinda não há avaliações
- Ckd. CKF 2020Documento20 páginasCkd. CKF 2020CristinaGheorgheAinda não há avaliações
- Growth and Development: A Multifactorial ProcessDocumento41 páginasGrowth and Development: A Multifactorial ProcessCristinaGheorgheAinda não há avaliações
- Heart Failure in ChildrenDocumento36 páginasHeart Failure in ChildrenCristinaGheorgheAinda não há avaliações
- Congenital Heart DiseaseDocumento83 páginasCongenital Heart DiseaseArleen MatincaAinda não há avaliações
- Immunodeficiencies - Dr. BergheaDocumento50 páginasImmunodeficiencies - Dr. BergheaCristinaGheorgheAinda não há avaliações
- Cystic fibrosis – an overviewDocumento60 páginasCystic fibrosis – an overviewArleen MatincaAinda não há avaliações
- ToxicologyDocumento73 páginasToxicologyMunteanu LauraAinda não há avaliações
- Heart Failure in ChildrenDocumento36 páginasHeart Failure in ChildrenCristinaGheorgheAinda não há avaliações
- Course 2 HIE 2020Documento42 páginasCourse 2 HIE 2020CristinaGheorgheAinda não há avaliações
- LECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)Documento57 páginasLECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)CristinaGheorgheAinda não há avaliações
- Course 2 CP 2020Documento51 páginasCourse 2 CP 2020CristinaGheorgheAinda não há avaliações
- Lecture 1 PDFDocumento53 páginasLecture 1 PDFMunteanu LauraAinda não há avaliações
- Arterial Hypertension in ChildrenDocumento48 páginasArterial Hypertension in ChildrenCristinaGheorgheAinda não há avaliações
- Anemia SDocumento42 páginasAnemia SCristinaGheorgheAinda não há avaliações
- Bladder TumorsDocumento17 páginasBladder TumorsCristinaGheorgheAinda não há avaliações
- Aki. Arf 2020Documento35 páginasAki. Arf 2020CristinaGheorgheAinda não há avaliações
- CystitisDocumento9 páginasCystitisCristinaGheorgheAinda não há avaliações
- Acute LeukemiaDocumento20 páginasAcute LeukemiaCristinaGheorgheAinda não há avaliações
- Bladder PathologyDocumento4 páginasBladder PathologyCristinaGheorgheAinda não há avaliações
- Clinical Toxicology: Class No. 4Documento50 páginasClinical Toxicology: Class No. 4CristinaGheorgheAinda não há avaliações
- Acute Gastroenteritis 2020Documento56 páginasAcute Gastroenteritis 2020CristinaGheorgheAinda não há avaliações
- Benign Prostate HypertrophyDocumento25 páginasBenign Prostate HypertrophyCristinaGheorgheAinda não há avaliações
- Bladder LithiasisDocumento5 páginasBladder LithiasisCristinaGheorgheAinda não há avaliações
- Clinical Toxicology: Class No. 5Documento74 páginasClinical Toxicology: Class No. 5CristinaGheorgheAinda não há avaliações
- Hand Foot Mouth Disease (HFMD) For TeachersDocumento2 páginasHand Foot Mouth Disease (HFMD) For Teachersalbeny j.pAinda não há avaliações
- Alveolar Osteitis A Comprehensive Review ofDocumento10 páginasAlveolar Osteitis A Comprehensive Review ofFakhrul ImamAinda não há avaliações
- Cellular Cancer TherapyDocumento208 páginasCellular Cancer TherapyneuralterapianetAinda não há avaliações
- 2nd Periodical TestDocumento11 páginas2nd Periodical TestGiYaIbarbiaAinda não há avaliações
- Route of Drug AdministrationDocumento3 páginasRoute of Drug AdministrationAjay SinghAinda não há avaliações
- Darwins Voyage PowerPoint For WebsiteDocumento38 páginasDarwins Voyage PowerPoint For WebsiteEko SujatmikoAinda não há avaliações
- PhysiologyDocumento2 páginasPhysiologyapi-19762967Ainda não há avaliações
- Anatomy and Physiology of the HeartDocumento56 páginasAnatomy and Physiology of the Heartamjad khan100% (1)
- Hippoboscidae Family Flies: Morphology, Life Cycle & ControlDocumento28 páginasHippoboscidae Family Flies: Morphology, Life Cycle & ControlAvitus Dastan CastoAinda não há avaliações
- ANTI OBESITY CAMPDocumento13 páginasANTI OBESITY CAMPgirishlambaAinda não há avaliações
- Prevalence of Sarcoptic Mange in Rabbits: A. Meenakshisundaram and T. AnnaDocumento6 páginasPrevalence of Sarcoptic Mange in Rabbits: A. Meenakshisundaram and T. AnnaAchmad NugrohoAinda não há avaliações
- Water Balance Laboratory HandoutDocumento8 páginasWater Balance Laboratory HandoutTheng.SethAinda não há avaliações
- Jurnal LepraDocumento20 páginasJurnal LepraCalvin AffendyAinda não há avaliações
- TABLE (Ascaris, Trichuris, and Enterobius)Documento3 páginasTABLE (Ascaris, Trichuris, and Enterobius)TRISHA MAE ORDONAAinda não há avaliações
- Thoracic WallDocumento12 páginasThoracic WallZainab NaffeeAinda não há avaliações
- Early Human DietsDocumento3 páginasEarly Human DietsDouglas CamposAinda não há avaliações
- Killer Whales (Orcas) Unsuccessful Births by Mother's NameDocumento2 páginasKiller Whales (Orcas) Unsuccessful Births by Mother's NameThe Orca Project Corp100% (1)
- Care Sheet - Axolotl (Ambystoma Mexicanum)Documento3 páginasCare Sheet - Axolotl (Ambystoma Mexicanum)John GamesbyAinda não há avaliações
- Rose - 2001 - Pesticides and Public Health Integrated Methods of Mosquito Management PDFDocumento7 páginasRose - 2001 - Pesticides and Public Health Integrated Methods of Mosquito Management PDFYrllan SincuráAinda não há avaliações
- Urine Culture Test: Tests and ProceduresDocumento2 páginasUrine Culture Test: Tests and ProceduresVikashKumarAinda não há avaliações
- What Is Dairy RanchingDocumento3 páginasWhat Is Dairy RanchingBright SamuelAinda não há avaliações