Escolar Documentos
Profissional Documentos
Cultura Documentos
Spinal Cord: Prof DR Nasaruddin Abdul Aziz
Enviado por
kyoko080 notas0% acharam este documento útil (0 voto)
71 visualizações54 páginasTítulo original
Anatomy Spine2
Direitos autorais
© Attribution Non-Commercial (BY-NC)
Formatos disponíveis
PPT, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
71 visualizações54 páginasSpinal Cord: Prof DR Nasaruddin Abdul Aziz
Enviado por
kyoko08Direitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato PPT, PDF, TXT ou leia online no Scribd
Você está na página 1de 54
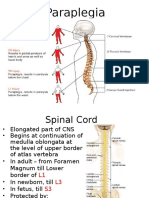
SPINAL CORD
PROF DR NASARUDDIN ABDUL AZIZ
Management & Science University
dr_nasaruddin@msu.edu.my
OBJECTIVES
• describe the external structure of the spinal
cord,
• draw and describe the internal structure of
the spinal cord,
• draw and describe the ascending and
descending tracts within the spinal cord,
• describe the meninges surrounding the
spinal cord,
• describe the blood supply of the spinal cord,
• explain the clinical correlations of &
applications related to the spinal cord
Gross Appearance
• Cylindrical in shape
• Foramen magnum L1/L2 (adult)
• L3 (newborn)
• Occupies upper ⅔ of vertebral canal
• Surrounded by 3 layers of meniges:
– dura mater
– arachnoid mater
– pia mater
• CSF in subarachnoid space
• Enlargements: cervical & lumbar
• Conus medullaris
• Filum termniale
• Anterior median fissure
• Posterior median sulcus
• 31 pairs of spinal nerves attached to it by
the anterior roots & posterior roots
Structure Of The Spinal Cord
Gray Matter
• H-shaped pillar with anterior & posterior gray
horns
• United by gray commissure containing the
central canal
• Lateral gray column (horn) present in
thoracic & upper lumbar segments
• Amount of gray matter related to the amount
of muscle innervated
• Consists of nerve cells, neuroglia, blood
vessels
Nerve cells in the anterior gray columns
• Large & multipolar
• Axons pass out in the anterior nerve roots
as α-efferents
• Smaller nerve cells are multipolar
• Axons pass out in anterior roots as ɣ-
efferents
Nerve cells in the posterior gray columns
• 4 nerve cell groups
• Substantia gelatinosa
– situated at the apex
– throughout the length of spinal cord
– composed mainly of Golgi Type II neurons
– receives afferent fibres concerning with pain,
temperature & touch from posterior root
• Nucleus proprius
– anterior to substantia gelatinosa
– present throughout the whole length of spinal
cord
– main bulk of cells in posterior gray column
– receives fibers from posterior white column
that are assoc with proprioception, 2-point
discrimination & vibration
• Nucleus dorsalis (Clark’s column)
– base of posterior column
– C8 – L3 / L4
– associated with proprioceptive endings
(neuromuscular spindles & tendon spindles)
• Visceral afferent nucleus
– lateral to nucleus dorsalis
– T1 – L3
– receives visceral afferent info
• Nerve cells in the lateral gray columns
• Formed by the intermediolateral group of
cells
• T1 – L2 / L3
• Cells give rise to preganglionic
sympathetic fibres
• In S2, S3, S4; they give rise to
preganglionic parasympathetic fibres
• The gray commissure & central canal
– connects the gray on each side
– central canal in the centre
– posterior gray commissure
– anterior gray commissure
– central canal present throughout
– superiorly continuous with the central canal of
medulla oblongata
– inferiorly, expands as terminal ventricle
– terminates within the root of filum terminale
White Matter
• Divided into
– anterior white column
– lateral white column
– posterior white column
• Consists of nerve fibres, neuroglia, blood
vessels
• White due to myelinated fibres
Tracts
• Ascending
• Descending
• Intersegmental
Ascending Tracts
• Fibres that ascend from spinal cord to
higher centres
• Conduct afferent information which may or
may not reach consciousness
• Information may be
– exteroceptive (pain, Tº, touch)
– proprioceptive (from muscles & joints)
Organization
• Ascending pathway that reach
consciousness consists of 3 neurons:
– 1st-order neuron
– 2nd-order neuron
– 3rd-order neuron
• Branch to reticular formation
(wakefulness)
• Branch to motor neurons (reflex activity)
• Lateral spinothalamic tract
– pain & Tº
• Anterior spinothalamic tract
– light (crude) touch & pressure
• Fasciculus cuneatus
• Fasciculus gracilis
– discriminatory touch, vibration, info from muscles &
joints
• Anterior spinocerebellar tract
• Posterior spinocerebellar tract
– unconscious info from muscles, joints, skin, subcut
• Spinotectal tract
– spinovisual reflexes
• Spinoreticular tract
– info from muscles, joints & skin to reticular
formation
• Spino-olivary tract
– indirect pathway to cerebellum
Lateral spinothalamic tract
• Pain & temp pathways
• 1st-order neurons
• Pain conducted by δ A-type fibres & C-type
fibres
• 2nd-order neurons
– decussate to the opposite side
– ends in thalamus (ventral posterolateral nucleus
• 3rd-order neurons
– ends in sensory area in postcentral gyrus
Anterior spinothalamic tracts
• Light (crude) touch & pressure pathways
Posterior white column
• Discriminative touch, vibratory sense,
conscious muscle joint sense (conscious
proprioception)
Posterior spinocerebellar tract
• Muscle joint sense pathways to
cerebellum
• Unconscious proprioception
• Muscle joint info from muscle spindles,
GTO, joint receptors of the trunk & lower
limbs
• Info is used by the cerebellum in the
coordination of movements & maintenance
of posture
Anterior spinocerebellar tract
• Majority of 2nd-order neurons cross to the
opposite side
• Enter cerebellum through superior
cerebellar peduncle
• Info from trunk, upper & lower limbs
• Also carries info from skin & subcut tissue
Descending Tracts
• Lower motor neurons
• Upper motor neurons
• Corticospinal tracts
– concerned with voluntary, discrete, skilled
movements
• Reticulospinal tract
– facilitates or inhibits voluntary movement or reflex
activity
• Tectospinal tract
– reflex postural movements in response to visual
stimuli
• Rubrospinal tract
– facilitates activity of flexor muscles & inhibits
activity of extensor muscles
• Vestibulospinal tract
– facilitates extensor muscles, inhibits flexor
muscles
Meninges
• Dura mater
• Arachnoid mater
• Pia mater
Dura mater
• Dense, strong fibrous membrane
• Encloses the spinal cord & cauda equina
• Continuous above with meningeal layer of
dura covering the brain
• Ends at the level of S2
• Separated from wall of vertebral canal by
the extradural space
• Contains loose areolar tissue & internal
vertebral venous space
Arachnoid mater
• Delicate impermeable membrane
• Lies between pia and dura mater
• Separated from pia mater by subarachnoid
space
• Continuous above with arachnoid mater
covering the brain
• Ends on filum terminale at level of S2
Pia mater
• Vascular membrane
• Closely covers spinal cord
• Thickened on either side between nerve
roots to form the ligamentum denticulatum
Blood supply
Arteries of the spinal cord
• Anterior spinal artery
• Posterior spinal artery
• Segmental spinal arteries
Anterior spinal artery
• Formed by the union of 2 arteries
• From vertebral artery
• Supply anterior ⅔ of spinal cord
Posterior spinal arteries
• Arise from vertebral artery or posterior
inferior cerebellar arteries (PICA)
• Descend close to the posterior roots
• Supply posterior ⅓ of spinal cord
Segmental spinal arteries
• Branches of arteries outside the vertebral
column
• Gives off the anterior & posterior radicular
arteries
• Great anterior medullary artery of
Adamkiewicz
• Arise from lateral intercostal artery or
lumbar artery at any level from T8 – L3
Clinical correlations
Spinal shock
• Follows acute severe damage to the spinal
cord
• All cord functions below the level of the
lesion become depressed or lost
• Sensory impairment and flaccid paralysis
occur
• Segmental spinal reflexes are depressed
• Persists for less than 24 hours (may be as
long as 1 – 4 weeks)
Poliomyelitis
• Acute viral infection of the neurones of
anterior gray column
• Motor nuclei of cranial nerves
• Death of motor neurone cells → paralysis
& wasting of muscles
• Muscles of lower limb more often affected
• Spinal anaesthesia
• Extradural anaesthesia
Você também pode gostar
- DSM 5 ChartDocumento2 páginasDSM 5 ChartJanie VandeBerg93% (27)
- The Making of Mess in Art Therapy PDFDocumento13 páginasThe Making of Mess in Art Therapy PDFRomina MarAinda não há avaliações
- Exercise 4 Frog Embryo 4mm 7mm 10mmDocumento23 páginasExercise 4 Frog Embryo 4mm 7mm 10mmrexartooz95% (19)
- 3-Ascending Tracts of Spinal CordDocumento28 páginas3-Ascending Tracts of Spinal Cordmuhammad altaf100% (2)
- Cns Anatomy & PhysiologyDocumento25 páginasCns Anatomy & PhysiologyAgatha TerenciaAinda não há avaliações
- Medical Surgical NursingDocumento110 páginasMedical Surgical Nursingarjetahoward100% (5)
- Neuro Case Study 1Documento2 páginasNeuro Case Study 1AngelaWise100% (1)
- Cook and Plisky - Balance, Posture and MovementDocumento57 páginasCook and Plisky - Balance, Posture and MovementFlávio Garrett100% (1)
- Practice TestDocumento11 páginasPractice TestOhTenThickeAinda não há avaliações
- Spinal Cord: Prof DR Nasaruddin Abdul AzizDocumento54 páginasSpinal Cord: Prof DR Nasaruddin Abdul AzizBJKines BjmcAinda não há avaliações
- The Spinal CordDocumento22 páginasThe Spinal Cordcy lifeAinda não há avaliações
- spinalcord-181202085959Documento95 páginasspinalcord-181202085959gonzalesmailyn85Ainda não há avaliações
- 14 The Central Nervous SystemDocumento61 páginas14 The Central Nervous SystemvanderphysAinda não há avaliações
- Spinal Cord: DR Ganesh Khemnar Assistant Professor Dept. of Anatomy BVDUMC, PuneDocumento43 páginasSpinal Cord: DR Ganesh Khemnar Assistant Professor Dept. of Anatomy BVDUMC, PunePraneetha NouduriAinda não há avaliações
- The Spinal CordDocumento59 páginasThe Spinal CordbegeerizikAinda não há avaliações
- Brain Anatomy: Diencephalon, Brain Stem and Medulla SpinalisDocumento36 páginasBrain Anatomy: Diencephalon, Brain Stem and Medulla SpinalisAngela FovinaAinda não há avaliações
- 5.spinal CordDocumento62 páginas5.spinal CordNishanth LakshmanAinda não há avaliações
- Spinal Cord AnatomyDocumento22 páginasSpinal Cord AnatomyAbdallah ElshayahAinda não há avaliações
- The Spinal Cord: DR - SatyaDocumento61 páginasThe Spinal Cord: DR - SatyacheckmateAinda não há avaliações
- Gross Anatomy of Spinal Cord: Dr. Normaizatul Afizah Ismail Normaizatul@unishams - Edu.myDocumento48 páginasGross Anatomy of Spinal Cord: Dr. Normaizatul Afizah Ismail Normaizatul@unishams - Edu.mykalppena naiduAinda não há avaliações
- Ascending TractsDocumento80 páginasAscending TractsAnonymous -Ainda não há avaliações
- Brain Stem: - Located BTWN The Cerebrum and The SCDocumento41 páginasBrain Stem: - Located BTWN The Cerebrum and The SCnkuligowskiAinda não há avaliações
- 2.spinal CordDocumento29 páginas2.spinal CordPraneethaAinda não há avaliações
- Ascending TractsDocumento42 páginasAscending TractsJustine Nyangaresi100% (2)
- Anatomy - Nervous System - Spinal Cord and Motor and Sensory PathwaysDocumento43 páginasAnatomy - Nervous System - Spinal Cord and Motor and Sensory PathwaysYAMINIPRIYAN100% (1)
- Spinal Cord Anatomy: Inha University Hospital Professor Yoon SHDocumento34 páginasSpinal Cord Anatomy: Inha University Hospital Professor Yoon SHEstrella RomAinda não há avaliações
- SPINAL NERVE Presentation Completed-2Documento51 páginasSPINAL NERVE Presentation Completed-2Sheikh Muhammad MuhallilAinda não há avaliações
- Spinal Cord and Nerve Plexii: by Dr. TDocumento20 páginasSpinal Cord and Nerve Plexii: by Dr. TthwisemanAinda não há avaliações
- Sensory: Sensory (Ascending) Spinal TractsDocumento24 páginasSensory: Sensory (Ascending) Spinal Tractsعبد الله الإمامAinda não há avaliações
- Week 3 Spinal Cord, Spinal NervesDocumento53 páginasWeek 3 Spinal Cord, Spinal NervesHephzibah JaporAinda não há avaliações
- Week 3 Spinal Cord, Spinal NervesDocumento53 páginasWeek 3 Spinal Cord, Spinal NervesCyril Jay G. OrtegaAinda não há avaliações
- DrMBA Medulla SpinalisDocumento25 páginasDrMBA Medulla SpinalisAyu FadhilahAinda não há avaliações
- Human Anatomy & Physiology: Spinal Cord, Spinal Nerves and Somatic ReflexesDocumento41 páginasHuman Anatomy & Physiology: Spinal Cord, Spinal Nerves and Somatic ReflexesSyarif MaulanaAinda não há avaliações
- SPINEDocumento27 páginasSPINEMadhavarao MaddisettyAinda não há avaliações
- 3.spinal CordDocumento46 páginas3.spinal CorddenekeAinda não há avaliações
- NervoussysteDocumento55 páginasNervoussysteaishabahaa03Ainda não há avaliações
- Spinal Cord AnatomyDocumento20 páginasSpinal Cord AnatomyrooparawatAinda não há avaliações
- Spinal CardDocumento10 páginasSpinal CardAsawara NoorAinda não há avaliações
- Brainstem (Yuni)Documento34 páginasBrainstem (Yuni)Ayi Abdul Basith100% (2)
- The Spinal Cord,, and Blood Supply To The BrainDocumento78 páginasThe Spinal Cord,, and Blood Supply To The BrainMartha MulusaAinda não há avaliações
- Spinal Cord - Gross AnatomyDocumento2 páginasSpinal Cord - Gross AnatomyshreyasAinda não há avaliações
- Spinal Cord and Spinal NervesDocumento67 páginasSpinal Cord and Spinal NervesRAVISHAinda não há avaliações
- Spinal CordDocumento60 páginasSpinal CordPiyush KumarAinda não há avaliações
- HNF 20 Cranial Nerves III, IV, VIDocumento23 páginasHNF 20 Cranial Nerves III, IV, VIthugsena39Ainda não há avaliações
- The Spinal Cord, Spinal Nerves, and Spinal ReflexesDocumento43 páginasThe Spinal Cord, Spinal Nerves, and Spinal ReflexesSyed Irfan ArifAinda não há avaliações
- The Midbrain and Important ConnectionsDocumento118 páginasThe Midbrain and Important ConnectionsBaguma MichaelAinda não há avaliações
- Anatomi Dan Fisiologi Sistem PersyarafanDocumento37 páginasAnatomi Dan Fisiologi Sistem PersyarafanAnonymous xfBKTQfAinda não há avaliações
- The Spinal Cord Medulla Spinalis: Introductory and Neuroanatomy LecturesDocumento24 páginasThe Spinal Cord Medulla Spinalis: Introductory and Neuroanatomy LecturesHumaira BadatAinda não há avaliações
- 2 NeuroanatomyDocumento60 páginas2 NeuroanatomyMeirina KhairatAinda não há avaliações
- Spinal CordDocumento38 páginasSpinal CordUrwah KhanAinda não há avaliações
- Chapter 13: The Spinal Cord, Spinal Nerves, and Spinal ReflexesDocumento43 páginasChapter 13: The Spinal Cord, Spinal Nerves, and Spinal ReflexesEzekiel ArtetaAinda não há avaliações
- Nervous tissue functions and cell typesDocumento34 páginasNervous tissue functions and cell typesSameer MohammedAinda não há avaliações
- ParaplegiaDocumento51 páginasParaplegiaChuah Wei HongAinda não há avaliações
- Wawa - Sistem Saraf PusatDocumento38 páginasWawa - Sistem Saraf PusatnuhaAinda não há avaliações
- Anatomy of BrainstemDocumento66 páginasAnatomy of BrainstemFitria OctavianiAinda não há avaliações
- Introduction to NeurologyDocumento105 páginasIntroduction to NeurologyaboubakarylwabukobaAinda não há avaliações
- Essentials of the Spinal Cord and Nervous SystemDocumento24 páginasEssentials of the Spinal Cord and Nervous Systemأمال داودAinda não há avaliações
- Anatomy, Neuroanatomy, and Vascular SupplyDocumento29 páginasAnatomy, Neuroanatomy, and Vascular SupplyNoemiPelilaLay-osBetatAinda não há avaliações
- Neuroscience: Ascending and Descending TracDocumento91 páginasNeuroscience: Ascending and Descending Trachazunga rayfordAinda não há avaliações
- Neuro AnatomyDocumento191 páginasNeuro Anatomysirima makuraAinda não há avaliações
- CerebrumDocumento26 páginasCerebrumsanthiyasandy100% (1)
- 8 محاضرات عصبيهDocumento35 páginas8 محاضرات عصبيهلوريس أبو الفتوحAinda não há avaliações
- Gambaran MeningesDocumento39 páginasGambaran MeningesPurnomo Ponco Nugroho100% (1)
- Spinal Cord Injury IntroductionDocumento243 páginasSpinal Cord Injury Introductionfahad100% (1)
- Ascending PathwaysDocumento54 páginasAscending Pathwaysrogegir407Ainda não há avaliações
- SDN vs DDN for MTrP PainDocumento5 páginasSDN vs DDN for MTrP PainludimilaGAinda não há avaliações
- Unit 13: Awareness of DementiaDocumento7 páginasUnit 13: Awareness of DementiaLiza GomezAinda não há avaliações
- Cerebral Palsy Procedure Reduces SpasticityDocumento7 páginasCerebral Palsy Procedure Reduces SpasticityAlvaro Perez HenriquezAinda não há avaliações
- Clinical Pathways in Stroke RehabilitationDocumento284 páginasClinical Pathways in Stroke RehabilitationArturo Valverde AmpaiAinda não há avaliações
- Regulation of RespirationDocumento21 páginasRegulation of RespirationSheeraz ShahzadAinda não há avaliações
- SEO Senses TestDocumento6 páginasSEO Senses TestAbbey MatosAinda não há avaliações
- Dokumen - Tips - 46201478 NCP Acute Abdominal Pain PDFDocumento5 páginasDokumen - Tips - 46201478 NCP Acute Abdominal Pain PDFmikhailAinda não há avaliações
- EXSC 224 Problems To PonderDocumento3 páginasEXSC 224 Problems To Ponderkimber brownAinda não há avaliações
- NCP Impaired Transfer AbilityDocumento2 páginasNCP Impaired Transfer AbilityMiar QuestAinda não há avaliações
- Identifying Imagery Types in Creative WritingDocumento8 páginasIdentifying Imagery Types in Creative WritingJilian MeiAinda não há avaliações
- The Importance of Diversity On Congitive NeuroscienceDocumento11 páginasThe Importance of Diversity On Congitive NeuroscienceMarlon ChaconAinda não há avaliações
- Instructional and Improvisational Models of Music Therapy With Adolescents Who Have Attention Deficit Hyperactivity Disorder (ADHD)Documento153 páginasInstructional and Improvisational Models of Music Therapy With Adolescents Who Have Attention Deficit Hyperactivity Disorder (ADHD)ywwonglpAinda não há avaliações
- All PSY Notes (Slides)Documento66 páginasAll PSY Notes (Slides)JessicaWuAinda não há avaliações
- Vision Screening Form DepedDocumento3 páginasVision Screening Form DepedAbigael Abac RiveraAinda não há avaliações
- Human Physiology I - 2022.02.01Documento5 páginasHuman Physiology I - 2022.02.01Charlie JohnsonAinda não há avaliações
- Speech and Communication DisordersDocumento3 páginasSpeech and Communication Disordersalessandra padulaAinda não há avaliações
- HMB200 Lecture 10 ASD Genetics 2020-21Documento56 páginasHMB200 Lecture 10 ASD Genetics 2020-21bluetooth opencvAinda não há avaliações
- Peripheral Nerve CME 17 DECDocumento4 páginasPeripheral Nerve CME 17 DECSwarup SonawaneAinda não há avaliações
- Bahan BrainDocumento7 páginasBahan BrainArwina Syazwani Binti GhazaliAinda não há avaliações
- CSF Cell Count: How The Test Is PerformedDocumento3 páginasCSF Cell Count: How The Test Is PerformedMars AqmalAinda não há avaliações
- Children With Special NeedsDocumento22 páginasChildren With Special NeedsNur AskinahAinda não há avaliações
- (10920684 - Neurosurgical Focus) Tuberculum Sellae MeningiomasDocumento6 páginas(10920684 - Neurosurgical Focus) Tuberculum Sellae MeningiomasputriAinda não há avaliações
- Sensory Processing Disorder (SPD)Documento1 páginaSensory Processing Disorder (SPD)sageAinda não há avaliações