Escolar Documentos
Profissional Documentos
Cultura Documentos
Artigo - Suplementacao de L-Arginina Potencializa A Hipotensao Pos Exercicios em Mulheres Idosas
Artigo - Suplementacao de L-Arginina Potencializa A Hipotensao Pos Exercicios em Mulheres Idosas
Enviado por
Jhuli CeconTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Artigo - Suplementacao de L-Arginina Potencializa A Hipotensao Pos Exercicios em Mulheres Idosas
Artigo - Suplementacao de L-Arginina Potencializa A Hipotensao Pos Exercicios em Mulheres Idosas
Enviado por
Jhuli CeconDireitos autorais:
Formatos disponíveis
L-ARGININE SUPPLEMENTATION IMPROVES POST-EXERCISE
HYPOTENSION IN ELDERLY WOMEN
SUPLEMENTAÇÃO DE L-ARGININA POTENCIALIZA A HIPOTENSÃO PÓS-EXERCÍCIO EM MULHERES IDOSAS Original Article
LA SUPLEMENTACIÓN DE L-ARGININA POTENCIALIZA LA HIPOTENSIÓN POST EJERCICIO EN MUJERES Artigo Original
Artículo Original
DE LA TERCERA EDAD
Juliano Casonatto1 ABSTRACT
(Physical Education Professional)
Daniele Mantovani Zago1 Introduction: L-Arginine supplementation increases plasma levels of nitric oxide (NO) metabolites, an
(Physical Education Professional) important mediator of peripheral dilatation. Therefore, L-Arginine supplementation can improve the duration
Daniel Massaharu Enokida1 and magnitude of post-exercise hypotension. Objectives: This study investigated the effects of L-Arginine su-
(Nutritionist) pplementation on post-exercise hypotension, femoral artery area and heart rate variability in elderly women.
Kamila Grandolfi1 Methods: Twenty prehypertensive and hypertensive adult female participants were divided (in a random and
(Physical Education Professional)
balanced manner) into two groups (placebo and L-arginine). The participants ingested eight grams of inert
Andreo Fernando Aguiar2
(Sport Professional) substance (placebo group) or eight grams of L-Arginine (L-arginine group), dissolved in water, 90 min prior to
the experimental session. The experimental session consisted of an isokinetic maximal strength test. Blood
1. Universidade Norte do Paraná pressure was measured using an oscillometric device (Omron MX3 Plus, Bannockburn, US) every 10 minutes for
(UNOPAR), Physiology and Physical 60 minutes after the experimental session. Femoral artery area (ultrasound) and heart rate variability were also
Activity Research and Study Group analyzed. Data underwent repeated measures (ANOVA) analysis and respective assumptions. Results: L-Arginine
(GEPEFAF), Health and Biological supplementation associated with exercise produced a significant decrease in systolic blood pressure [placebo
Sciences Center (CCBS), Londrina, vs L-Arginine] (p <0.05) at the “half-life” time point (90 minutes after supplementation) (141±12 vs 130±11
PR, Brazil.
mmHg) and 40 min. (146±13 vs 127±13 mmHg), 50 min. (145±20 vs 127±15 mmHg) and 60 min. (147±19 vs
2. Universidade Norte do Paraná
129±14mmHg) post-exercise. No significant differences were identified in femoral artery area and heart rate
(UNOPAR), Centro de Ciências
Biológicas e da Saúde (CCBS),
variability. Conclusion: Acute L-Arginine supplementation can increase post-exercise hypotension effects in
Londrina, PR, Brazil. elderly women. Additionally, acute L-Arginine supplementation is not related to either femoral artery area or
heart rate variability responses. Level of evidence I; Randomized clinical trial.
Correspondence:
Juliano Casonatto Keywords: Arterial pressure; Vasodilation; Arginine.
Rua Vereador Manoel de Oliveira
Branco, 91, Vila Rica. Londrina, RESUMO
PR, Brazil. 86025-170. Introdução: A suplementação de L-arginina aumenta os níveis plasmáticos dos metabólitos de óxido nítrico, um impor-
juliano2608@hotmail.com.br tante mediador da dilatação periférica. Dessa forma, é possível que a suplementação de L-arginina maximize a duração e a
magnitude dos efeitos hipotensores pós-exercício. Objetivos: O presente estudo investigou os efeitos da suplementação de
L-arginina na hipotensão pós-exercício, área da artéria femoral e variabilidade da frequência cardíaca em mulheres idosas.
Métodos: Vinte participantes, adultas, pré-hipertensas e hipertensas foram divididas (de modo aleatório e equilibrado)em
dois grupos (placebo e L-arginina). As participantes ingeriram oito gramas de substância inerte (grupo placebo) ou oito
gramas de L-arginina (grupo L-arginina), dissolvido em água, 90 min antes da realização da sessão experimental. A sessão
experimental consistia em um teste de força isocinética máxima. A pressão arterial foi aferida utilizando um dispositivo
oscilométrico (Omron MX3 Plus, Bannockburn, EUA) a cada 10 minutos, durante 60 minutos, após o término da sessão
experimental. Foram analisadas ainda a variabilidade da frequência cardíaca e a área da artéria femoral (ultrassom). Os
dados foram submetidos à análise de variância para medidas repetidas (ANOVA) e seus respectivos pressupostos. Resultados:
A suplementação de L-arginina associada ao exercício promoveu redução significativa da pressão arterial sistólica [placebo
vs. L-arginina] (p<0,05) no intervalo de “meia-vida” (90 minutos após a suplementação) (141±12 vs. 130±11 mmHg) e aos 40
min. (146±13 vs. 127±13 mmHg), 50 min. (145±20 vs. 127±15 mmHg) e 60 min. (147±19 vs. 129±14 mmHg) pós-exercício.
Não foram identificadas diferenças significativas na área da artéria femoral e na variabilidade da frequência cardíaca.
Conclusão: A suplementação aguda de L-arginina pode potencializar os efeitos hipotensores pós-exercício em mulheres
idosas. Além disso, a suplementação de L-arginina aguda não está associada às respostas de variabilidade da frequência
cardíaca ou da área da artéria femoral. Nível de evidência I; Ensaio clínico randomizado.
Descritores: Pressão arterial; Vasodilatação; Arginina.
RESUMEN
Introducción: La suplementación de L-arginina aumenta los niveles plasmáticos de los metabolitos de óxido nítrico, un
importante mediador de la dilatación periférica. De esa forma, es posible que la suplementación de L-arginina maximice
la duración y la magnitud de los efectos hipotensores post ejercicio. Objetivos: El presente estudio investigó los efectos de
la suplementación de L-arginina en la hipotensión post ejercicio, área de la arteria femoral y variabilidad de la frecuencia
cardíaca en mujeres de la tercera edad. Métodos: Veinte participantes, adultas, pre hipertensas e hipertensas fueron divi-
didas (de modo aleatorio y equilibrado) en dos grupos (placebo y L-arginina). Las participantes ingirieron ocho gramos
Rev Bras Med Esporte – Vol. 25, No 4 – Jul/Ago, 2019 333
de sustancia inerte (grupo placebo) u ocho gramos de L-arginina (grupo L-arginina), disuelta en agua, 90 minutos antes
de la realización de la sesión experimental. La sesión experimental consistía en un test de fuerza isocinética máxima. La
presión arterial fue medida utilizando un dispositivo oscilométrico (Omron MX3 Plus, Bannockburn, EE.UU.) a cada 10
minutos, durante 60 minutos, después del término de la sesión experimental. Fueron analizadas además la variabilidad
de la frecuencia cardíaca y el área de la arteria femoral (ultrasonido). Los datos fueron sometidos a análisis de variancia
para medidas repetidas (ANOVA) y sus respectivas premisas. Resultados: La suplementación de L-arginina asociada al
ejercicio promovió reducción significativa de la presión arterial sistólica [placebo vs. L-arginina] (p<0,05) en el intervalo de
“media vida” (90 minutos después de la suplementación) (141±12 vs. 130±11 mmHg) y a los 40 min. (146±13 vs. 127±13
mmHg), 50 min. (145±20 vs. 127±15 mmHg) y 60 min. (147±19 vs. 129±14 mmHg) post ejercicio. No fueron identificadas
diferencias significativas en el área de la arteria femoral ni en la variabilidad de la frecuencia cardíaca. Conclusión: La
suplementación aguda de L-arginina puede potencializar los efectos hipotensores post ejercicio en mujeres de la tercera
edad. Además, la suplementación de L-arginina aguda no está asociada a las respuestas de variabilidad de la frecuencia
cardíaca o del área de la arteria femoral. Nivel de evidencia I; Ensayo clínico aleatorizado.
Descriptores: Presión arterial; Vasodilatación; Arginina.
DOI: http://dx.doi.org/10.1590/1517-869220192504182865 Article received on 07/18/2017 accepted on 03/29/2019
INTRODUCTION METHODS
The social conditions and technological advances evidenced in the Participants
last century allowed a significant improvement in the health conditions After the sample size calculation (see statistical analysis), 20 physi-
of the population. Consequently, there has been a significant increase cally active elderly women (65-80 years old), who voluntarily participated
in life expectancy and an increase in the elderly population. In this in extension projects (general physical activities [functional exercises
scenario, infect-contagious diseases, which were responsible for high and stretching] offered to the community), were invited to compose
mortality rates, are no longer prevalent1. On the other hand, there is the present investigation. The inclusion criteria were: (1) nonsmoker,
a significant prevalence/incidence increase of chronic-degenerative (2) health musculoskeletal condition, (3) have not to use drugs that
diseases due to modern lifestyle characteristic. Among chronic-dege- potentiate or block muscle action, (4) have not to use medicines that
nerative diseases, systemic arterial hypertension and, consequently, increase blood flow, (5) have no surgeries at least six months, (6) have
cardiovascular diseases2. not used ergogenic supplements for at least six months, (7) have no
Physical activity practice is an important non-pharmacological disease or cardiac complication in the last three years, and (8) medical
resource for maintaining blood pressure control. Several studies have approval for physical exercise practice. All participants were previously
demonstrated that regular exercise promotes chronic blood pressure informed about the research objectives and procedures. They signed
(BP) reduction, through aerobic3 or resistance3 exercise. In addition, a free and informed consent form approved by the Research Ethics
there is still an acute reduction phenomenon called post-exercise Committee (protocol no. 28443714.0.0000.0108). All procedures were
hypotension (PEH), identified in both normotensive4 and hyperten- carried out in accordance with Helsinki Declare (1964).
sive5 individuals.
Different regulatory mechanisms can be related to BP changes. In Experimental Design
general, changes in cardiac contractility, microvessel density, arterial and The present study employed a randomized, double-blind experimen-
venous blood volume, heart thickness and morphology can modulate tal design with placebo group. Initially, all subjects were submitted to a
BP. Thus, the autonomic nervous system also plays an important role in quadriceps muscle isokinetic strength test familiarization. All participants
cardiovascular control, acting on heart rate, peripheral vascular resistance received instructions related to exercise technique and instruments. This
and consequently cardiac output and BP6. procedure was adopted to avoid potential learning effects and guarantee
The nitric oxide (NO) synthesis is another important process that must data reliability. Participants were divided randomly (using a random num-
be considered in relation to BP. NO plays an important role in increasing ber table - https://www.random.org/) into two groups (N = 10 per group):
blood flow, vasodilation, and blood perfusion7. NO can be produced Placebo (PLA) and ARG (ARG). The participants were submitted to femoral
in the mammalian organism or by the endogenous substrates such as artery doppler ultrasonography (performed by a specialized physician), into
L-Arginine (ARG) and L-Citrulline. Studies have shown that during the three moments: before ARG supplementation (moment 10 minutes [min].),
aging process there is a decrease in NO production and ARG (essential After ARG supplementation (80 min.), and immediately after performing
amino acid)8. This reduction is intrinsically related to physical exercise the isokinetic force test of the quadriceps muscle. Initially, participants
intolerance and cardiovascular risk factors9. Considering the importance were instructed to remain at rest for 30 min, they were supplemented with
of NO as a vasodilator, several pharmacological and nutritional therapies ARG or placebo (8g in a single dose) and kept seated at rest for 80 min.
have emerged recently10. After this, the participants were submitted to ultrasound examination and
Since ARG is the main endogenous substrate related to NO syn- isokinetic force test. HRV was continuously monitored. BP was monitored
thesis11, the ARG supplementation may play an important vasodilatory every 10 min intervals before (10, 20 and 30 min) and after (40, 50, 60, 70,
role, maximizing the already known post-exercise hypotensive effect, 80, 90, 100, 110, 120, 130, 140, 150, 160, 170,180 min.) supplementation.
becoming another important tool for the treatment and prevention of
hypertension. In this sense, the objective of the present study was to Familiarization Protocol
verify the impact of a single aerobic physical exercise session associated To avoid potential learning effects and to ensure the reliability, all
with ARG supplementation on BP, femoral artery area and heart rate participants were submitted to a familiarization session to receive te-
variability (HRV) in elderly women. chnique instructions related to isokinetic force test. Two familiarization
334 Rev Bras Med Esporte – Vol. 25, No 4 – Jul/Ago, 2019
training was carried out separated by at least 48 hours. This design was Kubios HRV software. The “pre”, “half-life” and “post” values were obtained
used to minimize the previous fatigue effects on strength tests and to by the mean of the moments, [10 and 20 min.]; [30, 40, 50, 60, 70, 80, 90,
guarantee maximum effort in each test. Each test was run three times 100, 110 and 120 min.]; [130, 140, 150, 160, 170 and 180 min], respectively.
during the familiarization phase. A 10 min recovery period was allowed
between trials. During all tests, the subjects were continuously monitored Food Control
and verbally encouraged. Participants were instructed to maintain their usual daily activities and
diet as well as to refrain from any strenuous activity and to avoid the rich
Anthropometry
nitrite/nitrate foods for three days before each session. A list describing
Anthropometric data were collected before the experimental ses- foods that should be avoided was distributed to simplify their dietary
sion. The body mass was evaluated with an electronic scale (Plenna choices. This list was developed based on nitrite/nitrate food estimates,
Acqua - São Paulo - Brazil). The portable wooden stadiometer was used as proposed by Griesenbeck16. Participants were also instructed to report
to stature measures. any adverse events. Participants did not report adverse events.
Arginine supplementation Statistical treatment
Subjects were supplemented with ARG (Sigma Aldrich®) or placebo
Assuming a standard deviation of 5mmHg17 for systolic BP, an alpha
(inert substance), in the same format. ARG was administered after 30
of 5%, and 80% of statistical power to detect a minimum difference of
min (8g – single dose) by the solution containing 300 ml of H2O. The
7mmHg17, 7 participants were required in each group.
tests were started at 90 min after supplementation (during half-life),
Independent Student’s t-test was applied for baseline comparisons.
considering ARG pharmacokinetic properties.
Mauchly’s test was applied to identify the data sphericity. In case of
Blood flow measurement sphericity breach, the Greenhouse-Geisser correction was applied.
All participants were submitted to a Doppler ultrasonography (Sys- Afterward, the data were submitted to variance analysis for repeated
tem FiVe; GE Medical Systems), performed by a specialized physician. measures. LSD post-hoc test was used for multiple comparisons. The P
Longitudinal femoral artery images were obtained by a linear matrix value <0.05 was adopted as statistically significant. Values are presented
(10-MHz) pulse doppler ultrasound probe. as mean and standard error. The data were analyzed with SPSS version 17.
Isokinetic Strength RESULTS
After 80 min of supplementation, all participants underwent to an The general characteristics (age, body mass, height, body mass index,
isokinetic evaluation (knee extensor and flexor muscles) of the dominant heart rate, systolic/diastolic BP and femoral artery area) are presented in Table 1.
limb by the isokinetic dynamometer (Biodex Medical Systems - 3 Isokinetic There were no baseline significant differences (P>0.05) between PLA and ARG.
Dynamometer, Long Island, NY). The participants were positioned on The systolic BP values were significantly different at the “half-life” [90
the equipment according to the manufacturer recommendations. The min after supplementation] (141 ± 12 vs 130 ± 11 mmHg) and at 40
subjects were instructed to perform three sets (10 repetitions; 60°/s [1.05
min. (146 ± 13 vs. 127 ± 13mmHg), 50 min. (145 ± 20 vs 127 ± 15mmHg)
rad.s-1]), applying recovery time (1 min) between the series. The move-
and 60 min. (147 ± 19 vs 129 ± 14 mmHg) post-exercise (PLA vs ARG,
ment angle was set at 90°. The test was performed after specific warming
respectively). Systolic BP remained higher at 10, 20, 30, and 40 min post-
(eight repetitions - 60º/s,) in which participants were instructed to do not
exercise for PLA and at 10 and 20 min for ARG compared to rest. There
perform the maximum effort. The dynamometer axis rotation was aligned
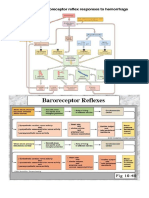
were no diastolic BP differences (Figure 1).
to the femoral epicondyle, and the resistance load was allocated two cen-
Figure 2 presents femoral artery area results for “pre”, “half-life” (90 min
timeters above the internal malleolus. Possible errors induced by gravity
were corrected based on the lower limb weight at 0º/s and calculated by after supplementation) and “post”. No statistically significant differences
the equipment software. The subjects were continuously monitored and were identified.
verbally encouraged by the evaluators. It was not allowed visual feedback. Figures 3 and 4 present the time (figure 3) and frequency (Figure 4) HRV
domains indicators. No statistically significant differences were identified.
Blood Pressure Measures
Resting BP was measured (every 10 min) by a pre-validated auto- DISCUSSION
mated monitor (Omron MX3 Plus, Bannockburn, USA)12. The subjects To the best of our knowledge, this is the first randomized, doub-
adopted the sitting position and the measurement was performed in the le-blind, placebo-controlled study that examined the acute effects of
left arm, following the American Heart Association13 recommendations. oral ARG supplementation on post-exercise pressure and autonomic
responses. It is worth mentioning that PEH is considered an important
Heart rate variability measurements
physiological phenomenon18, and may play a greater role in hypertension
HRV was monitored throughout the experimental session with a pre-
viously validated heart rate monitor (Polar - RS800CX, Kempele, Finland)14. Table 1. General characteristics of the sample.
The R-R interval ranges recorded on the equipment were transferred to ARG (N = 10) PLA (N = 10) P
a computer using Polar Precision Performance software (release 3.00, Age (years) 70,6 ± 2,2 72,5 ± 1,6 0,709
Kempele, Finland). The Fourier transform was used to quantify the low Body mass (kg) 62,9 ± 3,3 60,4 ± 2,1 0,538
(LF) and high frequency (HR) bands, according to the Task Force of the Height (cm) 153,2 ± 2,3 152,2 ± 1,1 0,699
European Society of Cardiology and the North American Society of Elec- BMI (kg∙m2) 27,1 ± 1,0 26,1 ± 0,7 0,620
trophysiology15 recommendations. The time domain analysis was obtained HR (bpm) 76,5 ± 3,5 70,3 ± 2,8 0,287
by the RMSSD indices (square root of the mean of successive squared Systolic BP (mmHg) 121,5 ± 6,0 124,3 ± 5,5 0,123
differences between adjacent R-Rs) and pNN50 (percentage of adjacent Diastolic BP (mmHg) 73,8,1 ± 1,7 75,8 ± 2,9 0,793
normal RR intervals with duration difference greater than 50ms). The time Femoral artery area (cm2) 0,45 ± 0,03 0,41 ± 0,02 0,327
and frequency domain analysis were performed every 10 minutes, by the ARG= L-Arginine Group; PLA= Placebo Group; BMI= Body mass index; HR= Heart rate; BP= Blood pressure.
Rev Bras Med Esporte – Vol. 25, No 4 – Jul/Ago, 2019 335
Figure 3. Time domains heart rate variability indicators.
HL= half-life; *P<0.05 vs rest; †P<0.05 vs L-arginine group.
Figure 1. Systolic and diastolic blood pressure changes.
Figure 2. Femoral artery area on “pre”, “half-life”, and post.
management since previous studies have shown that PEH magnitude
is correlated with chronic BP reductions19.
It is important to consider that ARG is the main amino acid related to the
NO synthesis11, consequently, ARG supplementation may play an important
vasodilatory role, although arginine is directly involved in protein synthesis,
ureagenesis, agmatine, creatine, polyamines, and proline productions20.
Data from experimental studies suggest that after oral administration, ARG
is extensively metabolized by arginase in the intestine and liver, limiting their
bioavailability as a NOS substrate and subsequent vasodilator function effects21.
Boger et al.22 conducted an experimental study using a stable ARG
isotope labeled and were able to show that only about 1% of the ARG
dose was being used as a nitric oxide synthase (NOS) substrate.
Thus, a high amino acid (8g) supplementation dose is justified in
the experimental protocol, trying to ensure that even a small part of the
supplement is used as a NOS substrate. This ARG dose has been previou-
sly used to promote vasodilator effect in elderly subjects23. According
to Böger24, single doses of 3 to 8 g of ARG appear to be safe and rarely
cause adverse events. On the other hand, single doses greater than 9 g
appear to be associated with gastrointestinal discomfort and nausea25. Figure 4. Frequency domains heart rate variability indicators.
336 Rev Bras Med Esporte – Vol. 25, No 4 – Jul/Ago, 2019
The hypothesis of the present study was that ARG supplementation of smooth muscle cells in continuous tone30. This fact suggests that
would maximize the PEH, characterized by the acute BP reduction after arterioles were more affected by NO than great vessels.
a single physical exercise or physical activity session26. In turn, the results To identify some effect related to the neuro-autonomic mechanism,
demonstrated that systolic BP remained lower post 40 min in the ARG HRV was investigated in different time/frequency domain components.
supplemented group compared to placebo. This result agree with the In this sense, there was no difference in any of the evaluated compo-
initial hypothesis since the ARG supplementation can increase the NO nents, suggesting that PEH identified is not strongly associated with
production27 and consequently peripheral vasodilation28. the central adjustments. Since HRV is an indirect autonomic nervous
On the other hand, no significant effects on diastolic BP were iden- system measure15, it was expected no significant changes in the HRV
tified in the present investigation. Studies investigating PEH has shown components, considering that HPE mechanisms were more strongly
smaller diastolic BP variations, several investigations demonstrate PEH associated with the peripheral adjustments.
only for systolic BP in hypertensive patients29. It is recommended that future studies add bioavailability markers
Another variable analyzed in the present investigation was the femoral of nitric oxide measurements, such as nitrite and nitrate. Additionally,
artery area. Considering that ARG is directly associated with NO synthesis, evaluation of other important mechanisms such as peripheral vascular
we expected the occurrence of vasodilation. However, this increase in the resistance and cardiac output may help in understand the ARG body
femoral artery area was not confirmed, contradicting the initial hypothesis. action. Finally, future research about ARG supplementation impact on
On the other hand, the vasodilation in large arteries may not occur PEH should be performed manipulating different exercise conditions,
systematically, since ARG supplementation may increase blood perfu- since exercise variables can change PEH.4, 5.
sion (reducing pressure) due to blood flow increase in arterioles and
capillaries7. The role of microcirculation on systemic vascular resistance CONCLUSION
is about 70% of the pressure gradient between arteries and veins. ARG supplementation may contribute to BP reduction after a single
The large arteries have architecture adapted to the shock absorption exercise session in hypertensive patients. In addition, ARG supplemen-
and blood volume accommodation every systole since the capillaries tation does not appear to promote femoral artery vasodilation and
arranged in a single layer of endothelial cells lining the basement autonomic nervous system changes.
membrane cannot receive blood at systemic pressures at the risk of
losing structural integrity. The required mechanical damping of the
pulse wave is promoted by arterioles equipped with one or two layers All authors declare no potential conflict of interest related to this article
AUTHORS’ CONTRIBUTIONS: Each author made significant individual contributions to this manuscript. JC (0000-0001-5397-5694)*: design, writing of the article, data interpretation,
and review; DMZ (0000-0003-3444-4323)*: writing, critical review, and intellectual concept; DME (0000-0001-5382-8360)*: writing and critical review; KG (0000-0002-8286-6072)*:
writing and critical review; AFA (0000-0003-3337-2444)* design and critical review. *ORCID (Open Researcher and Contributor ID).
REFERÊNCIAS
1. Campolina AG, Adami F, Santos JL, Lebrao ML. [The health transition and changes in healthy life 16. Griesenbeck JS, Steck MD, Huber JC, Jr., Sharkey JR, Rene AA, Brender JD. Development of estimates of
expectancy in the elderly population: possible impacts of chronic disease prevention]. Cadernos de dietary nitrates, nitrites, and nitrosamines for use with the Short Willet Food Frequency Questionnaire.
saude publica. 2013;29(6):1217-29. Nutrition journal. 2009;8:16.
2. Vidigal Fde C, Ribeiro AQ, Babio N, Salas-Salvado J, Bressan J. Prevalence of metabolic syndrome 17. Casonatto J, Tinucci T, Dourado AC, Polito M. Cardiovascular and autonomic responses after exercise
and pre-metabolic syndrome in health professionals: LATINMETS Brazil study. Diabetology & sessions with different intensities and durations. Clinics. 2011;66(3):453-8.
metabolic syndrome. 2015;7:6. 18. Halliwill JR, Buck TM, Lacewell AN, Romero SA. Postexercise hypotension and sustained postexercise
3. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. vasodilatation: what happens after we exercise? Exp Physiol. 2013;98(1):7-18.
J Am Heart Assoc. 2013;2(1):e004473. 19. Moreira SR, Cucato GG, Terra DF, Ritti-Dias RM. Acute blood pressure changes are related to chronic
4. Jones H, George K, Edwards B, Atkinson G. Is the magnitude of acute post-exercise hypotension mediated effects of resistance exercise in medicated hypertensives elderly women. Clin Physiol Funct Imaging.
by exercise intensity or total work done? Eur J Appl Physiol. 2007;102(1):33-40. 2016;36(3):242-8.
5. Pescatello LS, Guidry MA, Blanchard BE, Kerr A, Taylor AL, Johnson AN, et al. Exercise intensity alters 20. Wu G, Morris SM, Jr. Arginine metabolism: nitric oxide and beyond. The Biochemical journal. 1998;336
postexercise hypotension. J Hypertens. 2004;22(10):1881-8. (Pt 1):1-17.
6. Vanderlei LCM, Pastre CM, Hoshi HA, Carvalho TD, Godoy MF. Noções básicas de variablidade da frequência 21. Morris SM, Jr. Enzymes of arginine metabolism. J Nutr. 2004;134(10 Suppl):2743S-7S; discussion 65S-67S.
cardíaca e sua aplicabilidade clínica. Rev Bras Cir Cardiovasc. 2009;24(2):205-17.
22. Boger RH, Tsikas D, Bode-Boger SM, Phivthong-Ngam L, Schwedhelm E, Frolich JC. Hypercholesterolemia
7. Alvares TS, Conte-Junior CA, Silva JT, Paschoalin VM. Acute L-Arginine supplementation does not increase
impairs basal nitric oxide synthase turnover rate: a study investigating the conversion of L-[guanidino-(15)
nitric oxide production in healthy subjects. Nutrition & metabolism. 2012;9(1):54.
N(2)]-arginine to (15)N-labeled nitrate by gas chromatography--mass spectrometry. Nitric oxide : biology
8. Sindler AL, Fleenor BS, Calvert JW, Marshall KD, Zigler ML, Lefer DJ, et al. Nitrite supplementation reverses and chemistry. 2004;11(1):1-8.
vascular endothelial dysfunction and large elastic artery stiffness with aging. Aging cell. 2011;10(3):429-37.
23. Bode-Boger SM, Muke J, Surdacki A, Brabant G, Boger RH, Frolich JC. Oral L-arginine improves endothelial
9. Quyyumi AA, Dakak N, Andrews NP, Husain S, Arora S, Gilligan DM, et al. Nitric oxide activity in the function in healthy individuals older than 70 years. Vascular medicine. 2003;8(2):77-81.
human coronary circulation. Impact of risk factors for coronary atherosclerosis. The Journal of clinical
24. Boger RH. The pharmacodynamics of L-arginine. J Nutr. 2007;137(6 Suppl 2):1650S-5S.
investigation. 1995;95(4):1747-55.
25. Grimble GK. Adverse gastrointestinal effects of arginine and related amino acids. The Journal of nutrition.
10. Petroczi A, Naughton DP. Potentially fatal new trend in performance enhancement: a cautionary note
on nitrite. Journal of the International Society of Sports Nutrition. 2010;7:25. 2007;137(6 Suppl 2):1693S-701S.
11. Cynober L, Boucher JL, Vasson MP. Arginine metabolism in mammals. J Nutr Biochemistry. 1995;6(8):402-13. 26. Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA, et al. American College of Sports
Medicine position stand. Exercise and hypertension. Medicine and science in sports and exercise.
12. Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron MX3 Plus oscillometric blood
2004;36(3):533-53.
pressure monitoring device according to the European Society of Hypertension international protocol.
Blood Press Monit. 2005;10(3):165-8. 27. Nichols K, Staines W, Rubin S, Krantis A. Distribution of nitric oxide synthase activity in arterioles and
venules of rat and human intestine. The American journal of physiology. 1994;267(2 Pt 1):G270-5.
13. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure
measurement in humans and experimental animals: part 1: blood pressure measurement in humans: 28. Tang JE, Lysecki PJ, Manolakos JJ, MacDonald MJ, Tarnopolsky MA, Phillips SM. Bolus arginine supple-
a statement for professionals from the Subcommittee of Professional and Public Education of the mentation affects neither muscle blood flow nor muscle protein synthesis in young men at rest or after
American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697-716. resistance exercise. The Journal of nutrition. 2011;141(2):195-200.
14. Quintana DS, Heathers JA, Kemp AH. On the validity of using the Polar RS800 heart rate monitor for 29. Costa JBY, Gerage AM, Gonçalves CGS, Pina FLC, Polito MD. Influence of the training status on the
heart rate variability research. Eur J Appl Physiol. 2012;112(12):4179-80. blood pressure behavior after a resistance training session in hypertensive older females. Rev Bras
15. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force Med Esporte. 2010;16(2):103-6.
of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. 30. Kaiser SE. Contribuição do estudo da microcirculação à fisiopatologia da hipertensão arterial. Revista
Circulation. 1996;93(5):1043-65. HUPE. 2011;10(3):31-8.
Rev Bras Med Esporte – Vol. 25, No 4 – Jul/Ago, 2019 337
Você também pode gostar
- Suporte Avançado de Vida em PediatriaDocumento29 páginasSuporte Avançado de Vida em PediatriaMayara MedeirosAinda não há avaliações
- Aula 01 - Monitorização HemodinâmicaDocumento38 páginasAula 01 - Monitorização HemodinâmicaFabio CorreiaAinda não há avaliações
- Apostila Ecg Versão 2018Documento12 páginasApostila Ecg Versão 2018Anonymous n4gtOaochAinda não há avaliações
- Prova 5 Turma 5Documento2 páginasProva 5 Turma 5Luzivania Cabral100% (2)
- APG 8 - Ciclo CardíacoDocumento9 páginasAPG 8 - Ciclo CardíacoSabrina XavierAinda não há avaliações
- Influence of Aerobic Exercise Training On Cardiovascular and Endocrine Inflammatory Biomarkers in Hypertensive Postmenopausal WomenDocumento7 páginasInfluence of Aerobic Exercise Training On Cardiovascular and Endocrine Inflammatory Biomarkers in Hypertensive Postmenopausal WomenNemo SecretAinda não há avaliações
- Research Article: Martin Burtscher, Fritz Brunner, Martin Faulhaber, Barbara Hotter and Rudolf LikarDocumento9 páginasResearch Article: Martin Burtscher, Fritz Brunner, Martin Faulhaber, Barbara Hotter and Rudolf LikarGospodin CovekAinda não há avaliações
- WongDocumento5 páginasWongtalleresccorporal5Ainda não há avaliações
- Pre-Post Test Design With Total Sampling Technique, The Sample Size in This Study WasDocumento2 páginasPre-Post Test Design With Total Sampling Technique, The Sample Size in This Study Wasfirda ayuAinda não há avaliações
- Effects of Ace Inhibitors and Angiotensin Type 1.1266Documento1 páginaEffects of Ace Inhibitors and Angiotensin Type 1.1266Anett Pappné LeppAinda não há avaliações
- Anggina PectorisDocumento18 páginasAnggina PectorisHairunisa 0049Ainda não há avaliações
- A Red Wine Vinegar Beverage Can Inhibit The Renin-Angiotensin SystemDocumento3 páginasA Red Wine Vinegar Beverage Can Inhibit The Renin-Angiotensin SystemArielLunaAinda não há avaliações
- KafeinDocumento2 páginasKafeinPrayoga SiraitAinda não há avaliações
- DR - Risky Ika Riani Ppds I Gizi KlinikDocumento20 páginasDR - Risky Ika Riani Ppds I Gizi KlinikRisky RianiAinda não há avaliações
- Jurnal Gizor 1Documento18 páginasJurnal Gizor 1'Fika' Rafika KurniasihAinda não há avaliações
- Effect of Watermelon (Citrullus Lanatus) On Pulse Rate and Blood Pressure in Healthy IndividualsDocumento4 páginasEffect of Watermelon (Citrullus Lanatus) On Pulse Rate and Blood Pressure in Healthy IndividualsAyu WidiartiAinda não há avaliações
- Effect of Sacubitril/Valsartan On Exercise-Induced Lipid Metabolism in Patients With Obesity and HypertensionDocumento8 páginasEffect of Sacubitril/Valsartan On Exercise-Induced Lipid Metabolism in Patients With Obesity and HypertensionAnonymous dAS0SxsXijAinda não há avaliações
- Pre-Exercise Arginine Supplementation Increases Time To Exhaustion in Elite Male WrestlersDocumento5 páginasPre-Exercise Arginine Supplementation Increases Time To Exhaustion in Elite Male WrestlersAndrei ChirilaAinda não há avaliações
- Nutrition, Metabolism & Cardiovascular DiseasesDocumento8 páginasNutrition, Metabolism & Cardiovascular DiseasesDebora AlvesAinda não há avaliações
- Medicine The American Journal of Sports: Scapular Kinematics During Supraspinatus Rehabilitation ExerciseDocumento10 páginasMedicine The American Journal of Sports: Scapular Kinematics During Supraspinatus Rehabilitation ExerciseHelga Marlene Navarro ChávezAinda não há avaliações
- Peripheral Heart Action (PHA) Training As A Valid Substitute To High Intensity Interval Training To Improve Resting Cardiovascular Changes and Autonomic Adaptation Piras201Documento11 páginasPeripheral Heart Action (PHA) Training As A Valid Substitute To High Intensity Interval Training To Improve Resting Cardiovascular Changes and Autonomic Adaptation Piras201jojoAinda não há avaliações
- 2014 Cerda-Kohler Et Al, Effects of Continuous and Intermittent Endurance Exercise in Autonomic Balance, Rating Perceived Exertion and Blood Lactate Levels in Healthy SubjectsDocumento6 páginas2014 Cerda-Kohler Et Al, Effects of Continuous and Intermittent Endurance Exercise in Autonomic Balance, Rating Perceived Exertion and Blood Lactate Levels in Healthy SubjectsHugo Cerda KohlerAinda não há avaliações
- Foot Massage Terhadap Perubahan Tekanan DarahDocumento1 páginaFoot Massage Terhadap Perubahan Tekanan DarahAnonymous WIgZWcoFAinda não há avaliações
- Vranish 2016Documento7 páginasVranish 2016Jenifer de OliveiraAinda não há avaliações
- TRADUÇAODocumento1 páginaTRADUÇAOAnderson SiprianoAinda não há avaliações
- 1 s2.0 S2174204921001586 MainDocumento8 páginas1 s2.0 S2174204921001586 MainPedro HenriqueAinda não há avaliações
- Caffeine Vs Caffeine-Free Sports Drink Effects On Urine Production - Wemple 1997Documento7 páginasCaffeine Vs Caffeine-Free Sports Drink Effects On Urine Production - Wemple 1997Yo Vivo Fit Pablo y KarlaAinda não há avaliações
- Adenosine 5 - Triphosphate (ATP) Supplements Are1550-2783-9-16Documento9 páginasAdenosine 5 - Triphosphate (ATP) Supplements Are1550-2783-9-16mononoketangqihotmail.comAinda não há avaliações
- Citrulline, Arginine and High Intensity Exercise PerformanceDocumento2 páginasCitrulline, Arginine and High Intensity Exercise PerformanceLuis Castro XtrmAinda não há avaliações
- ClofibrateDocumento1 páginaClofibrateChristianHanjokarAinda não há avaliações
- Jurnal GerontikDocumento3 páginasJurnal GerontikCarla NasbarAinda não há avaliações
- No Effect of Short-Term Arginine Supplementation On Nitric Oxide Production, Metabolism and Performance in Intermittent Exercise in AthletesDocumento7 páginasNo Effect of Short-Term Arginine Supplementation On Nitric Oxide Production, Metabolism and Performance in Intermittent Exercise in AthletesArthurAinda não há avaliações
- Paccotti 2005Documento10 páginasPaccotti 2005Lucas CardosoAinda não há avaliações
- Net Notes CardioDocumento9 páginasNet Notes CardioJess PeltraAinda não há avaliações
- Bove 1979Documento8 páginasBove 1979Arthur PiresAinda não há avaliações
- Pengaruh Aktivitas Fisik Submaksimal (Rockport 1-Mile Walk Berolahraga Dan Yang Tidak Rutin BerolahragaDocumento4 páginasPengaruh Aktivitas Fisik Submaksimal (Rockport 1-Mile Walk Berolahraga Dan Yang Tidak Rutin BerolahragaOla SunAinda não há avaliações
- OrnitinaDocumento6 páginasOrnitinaNutricionista Lisa AfonsoAinda não há avaliações
- 10 1016@j Medcle 2016 11 016 PDFDocumento6 páginas10 1016@j Medcle 2016 11 016 PDFlabibah mahmudaAinda não há avaliações
- Exercise Is A Type of Physical Activity Consisting of Planned, Structured, and Repetitive BodilyDocumento3 páginasExercise Is A Type of Physical Activity Consisting of Planned, Structured, and Repetitive BodilyTiara Grhanesia DenashuryaAinda não há avaliações
- Umj 1x Dovangiova 3330 1 ManuskripDocumento8 páginasUmj 1x Dovangiova 3330 1 ManuskripNursaniahAinda não há avaliações
- Efeito Anti-Hipertensivo Do Exercicio The Anti-HypDocumento9 páginasEfeito Anti-Hipertensivo Do Exercicio The Anti-HypRicardo Tavares ArrudaAinda não há avaliações
- 2000 Adrenergic and Reflex Abnormalities in Obesity-Related HypertensionDocumento5 páginas2000 Adrenergic and Reflex Abnormalities in Obesity-Related HypertensionFerroBemAinda não há avaliações
- Perubahan Tekanan Darah Sebelum Dan Sesudah Pemberian Aromaterapi Pada Pasien Hipertensi Di Wilayah Kerja Puskesmas Jati Kabupaten KudusDocumento9 páginasPerubahan Tekanan Darah Sebelum Dan Sesudah Pemberian Aromaterapi Pada Pasien Hipertensi Di Wilayah Kerja Puskesmas Jati Kabupaten KudusNafik MunaAinda não há avaliações
- Parkinsonism and Related Disorders: David A. Low, Ekawat Vichayanrat, Valeria Iodice, Christopher J. MathiasDocumento5 páginasParkinsonism and Related Disorders: David A. Low, Ekawat Vichayanrat, Valeria Iodice, Christopher J. MathiasRafael Yokoyama FecchioAinda não há avaliações
- Effects of Endurance Training On Baroreflex Sensitivity and Blood Pressure in BorderliDocumento6 páginasEffects of Endurance Training On Baroreflex Sensitivity and Blood Pressure in BorderliMilenckaVidalConsiglieriAinda não há avaliações
- Exercise Effects On Cardiac Size and Left VentricularDocumento7 páginasExercise Effects On Cardiac Size and Left Ventricularmarielle.jobsAinda não há avaliações
- Aanalisis Jurnal Hematologi)Documento7 páginasAanalisis Jurnal Hematologi)Larassati LarasAinda não há avaliações
- The Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesDocumento7 páginasThe Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesZINATUL WIDADAinda não há avaliações
- Postprandial Light Physical Activity Blunts The Blood Glucose IncreaseDocumento3 páginasPostprandial Light Physical Activity Blunts The Blood Glucose IncreaseRemusLupinnAinda não há avaliações
- Influence of Brisk Walking Exercise On Blood Pressure Among Essential Hypertension PatientsDocumento6 páginasInfluence of Brisk Walking Exercise On Blood Pressure Among Essential Hypertension PatientsDiman MantoAinda não há avaliações
- 1 SMDocumento9 páginas1 SMsonia zhaharaAinda não há avaliações
- Effects of Hyperoxia On Skeletal Muscle Carbohydrate Metabolism During Transient and Steady-State ExerciseDocumento7 páginasEffects of Hyperoxia On Skeletal Muscle Carbohydrate Metabolism During Transient and Steady-State ExerciseNdelooDOnkAinda não há avaliações
- Ultra-Long-Distance Running and The Liver : U/L) To Day 19 (MeanDocumento5 páginasUltra-Long-Distance Running and The Liver : U/L) To Day 19 (MeanBilel ChefiratAinda não há avaliações
- Postexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State CyclingDocumento10 páginasPostexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State Cyclingnuttela ismeAinda não há avaliações
- JHH 2013 121Documento5 páginasJHH 2013 121adri20121989Ainda não há avaliações
- Heart Rate and Lower Limb Muscle Activity On Cycle ErgometerDocumento6 páginasHeart Rate and Lower Limb Muscle Activity On Cycle ErgometerVITOR PEREZAinda não há avaliações
- Article About Drug CardiovascularDocumento8 páginasArticle About Drug CardiovascularhandiAinda não há avaliações
- Reflex Effect of Skeletal Muscle MechanoreceptorDocumento9 páginasReflex Effect of Skeletal Muscle MechanoreceptorMateus José ArrudaAinda não há avaliações
- Nitric Oxide: S. Fernández Vallinas, N. López Carreras, M. Miguel, A. AleixandreDocumento3 páginasNitric Oxide: S. Fernández Vallinas, N. López Carreras, M. Miguel, A. AleixandreandratrifuAinda não há avaliações
- Effects of 40 Days of Pranayama Training in Hypertensive SubjectsDocumento5 páginasEffects of 40 Days of Pranayama Training in Hypertensive SubjectsnurindahwarAinda não há avaliações
- Comparison of The Subacute Hemodynamic Effects of Atenolol, Propranolol, Pindolol, and NebivololDocumento12 páginasComparison of The Subacute Hemodynamic Effects of Atenolol, Propranolol, Pindolol, and NebivololNiluh ItaAinda não há avaliações
- The Antioxidant Effects of Green Tea Reduces Blood Pressure and Sympathoexcitation in An Experimental Model of HypertensionDocumento7 páginasThe Antioxidant Effects of Green Tea Reduces Blood Pressure and Sympathoexcitation in An Experimental Model of Hypertensionpene asoyAinda não há avaliações
- Influence of Short-Term Exercise On Serum Leptin Concentration in The HorseDocumento8 páginasInfluence of Short-Term Exercise On Serum Leptin Concentration in The HorseparavelloAinda não há avaliações
- New Physiological Approach To Control Essenti HypertensionDocumento9 páginasNew Physiological Approach To Control Essenti HypertensionsandeepAinda não há avaliações
- Artigo Blog - TV e Comer Mais!Documento14 páginasArtigo Blog - TV e Comer Mais!Jhuli CeconAinda não há avaliações
- 29.11.18 Conhecimento Dos PEF Na Prescrição Do Exercício Aeróbico L1 - ARTIGO 188634 - RBME V24 N6 - 12 11 2018 PDFDocumento6 páginas29.11.18 Conhecimento Dos PEF Na Prescrição Do Exercício Aeróbico L1 - ARTIGO 188634 - RBME V24 N6 - 12 11 2018 PDFBruno SousaAinda não há avaliações
- UK Openhrt-2016-000519 TradDocumento5 páginasUK Openhrt-2016-000519 TradJhuli CeconAinda não há avaliações
- Piepoli2010 Europe TradDocumento18 páginasPiepoli2010 Europe TradJhuli CeconAinda não há avaliações
- Arab Countries 12913 2015 Article 1183 TraducaoDocumento10 páginasArab Countries 12913 2015 Article 1183 TraducaoJhuli CeconAinda não há avaliações
- Hipertensão PortalDocumento38 páginasHipertensão PortalAna Beatriz FernandesAinda não há avaliações
- Cardio Dilatado FelipeDocumento3 páginasCardio Dilatado FelipeRicardo CostaAinda não há avaliações
- Vter9 Fi Img 03Documento1 páginaVter9 Fi Img 03zavaAinda não há avaliações
- 23034c-DC-NovasRecomend Parada CardioRespDocumento7 páginas23034c-DC-NovasRecomend Parada CardioRespNadiana InocenteAinda não há avaliações
- Ficha Formativa12Documento6 páginasFicha Formativa12Sandra CoutoAinda não há avaliações
- Questões Fisiologia CardiovascularDocumento2 páginasQuestões Fisiologia Cardiovascularstephanie moreiraAinda não há avaliações
- Iam - AulaDocumento35 páginasIam - AulaRenata AlmeidaAinda não há avaliações
- Doenças Da Valva MitralDocumento50 páginasDoenças Da Valva MitralGustavo BarretoAinda não há avaliações
- E-Book Unidade 2Documento87 páginasE-Book Unidade 2Bons VentosAinda não há avaliações
- ExamenDocumento151 páginasExamenNatalia BuruianAinda não há avaliações
- Protocolo de Encaminhamento para Cirurgia VascularDocumento12 páginasProtocolo de Encaminhamento para Cirurgia VascularAdalbertoAinda não há avaliações
- Curso de Enfermagem em CardiologiaDocumento50 páginasCurso de Enfermagem em CardiologiagilbertonascimentoAinda não há avaliações
- Anatomia HumanaDocumento6 páginasAnatomia HumanaDaniel de OliveiraAinda não há avaliações
- Trabalho AteroscleroseDocumento8 páginasTrabalho AteroscleroseMarcio CardosoAinda não há avaliações
- Fisiologia CardiovascularDocumento36 páginasFisiologia CardiovascularCamila MartinsAinda não há avaliações
- Sistema CardiovascularDocumento5 páginasSistema CardiovascularLívia MirandaAinda não há avaliações
- 4 - Aspectos Contemporâneos Da Intervenção Coronária Percutânea No Tratamento Eletivo de Estenoses Localizadas No Tronco Não-Protegido Da Arteria Coronária EsquerdaDocumento12 páginas4 - Aspectos Contemporâneos Da Intervenção Coronária Percutânea No Tratamento Eletivo de Estenoses Localizadas No Tronco Não-Protegido Da Arteria Coronária EsquerdaLarissa BrandãoAinda não há avaliações
- Angioplastia e TranplanteDocumento37 páginasAngioplastia e TranplantePaibra DianaAinda não há avaliações
- O Que É ChoqueDocumento4 páginasO Que É ChoqueLainonaSpAinda não há avaliações
- (343028439) Sistema CirculatórioDocumento40 páginas(343028439) Sistema CirculatórioYasmin SantosAinda não há avaliações
- Medicina Interna Módulo 4Documento25 páginasMedicina Interna Módulo 4lbj23ar12Ainda não há avaliações
- TICS - Andreza Lúcia AVCDocumento4 páginasTICS - Andreza Lúcia AVCAndreza LuciaAinda não há avaliações
- Ressonância Magnética Cardíaca - Abono de FaltaDocumento10 páginasRessonância Magnética Cardíaca - Abono de Faltamarianalaranjeira27Ainda não há avaliações
- Linha de Cuidado Do Infarto Agudo Do MiocárdioDocumento4 páginasLinha de Cuidado Do Infarto Agudo Do MiocárdioPaulaAinda não há avaliações
- Electrocardiograma - Execuçao e InterpretaçaoDocumento45 páginasElectrocardiograma - Execuçao e InterpretaçaoHugo NogueiraAinda não há avaliações