Escolar Documentos
Profissional Documentos
Cultura Documentos
Creutzfeldt-Jakob Disease. Literature Review Based On Three Case Reports. 2022
Enviado por
Mariano David Díaz GambiniTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Creutzfeldt-Jakob Disease. Literature Review Based On Three Case Reports. 2022
Enviado por
Mariano David Díaz GambiniDireitos autorais:
Formatos disponíveis
Dement Neuropsychol 2022 December;16(4):367-372 Views & Reviews
https://doi.org/10.1590/1980-5764-DN-2021-0107
Creutzfeldt-Jakob disease:
literature review based on three case reports
Amandha Alencar Maia Carneiro1 , Mateus Aragão Esmeraldo1 ,
David Elison de Lima e Silva2 , Espártaco Moraes Lima Ribeiro1,2
ABSTRACT. Creutzfeldt-Jakob disease (CJD) is one of the transmissible spongiform encephalopathies that lead to rapidly
progressive dementia. CJD has a low prevalence, and the average survival is only 1 year after the onset of symptoms. As the
patients with CJD develop rapidly progressive dementia, associated with myoclonus, visual or cerebellar problems, pyramidal
or extrapyramidal features, and akinetic mutism, the hypothesis of CJD must be raised. Classic magnetic resonance imaging
(MRI) findings are hypersignals in the caudate nucleus, putamen, and cortical region. CJD must be considered a differential
diagnosis of other types of dementia, and there is no effective treatment for this disease. In this article, we present a literature
review based on the report of three cases of the sporadic form of this disease.
Keywords: Creutzfeldt-Jakob Syndrome; Prion Diseases; Myoclonus.
DOENÇA DE CREUTZFELDT-JAKOB: REVISÃO DA LITERATURA BASEADA NO RELATO DE TRÊS CASOS
RESUMO. A doença de Creutzfeldt-Jakob (DCJ) faz parte do grupo das encefalopatias espongiformes transmissíveis que levam
a um quadro de demência rapidamente progressiva. A DCJ possui baixa prevalência, e a sobrevida média é de apenas um ano
após o início dos sintomas. Diante de um paciente com demência rapidamente progressiva, associada a mioclonias, alterações
visuais ou cerebelares, sinais piramidais ou extrapiramidais e mutismo acinético, a hipótese de DCJ deve ser levantada.
Os achados clássicos na ressonância magnética são os hipersinais em núcleo caudado, putâmen e região cortical. A DCJ deve
ser considerada como um diagnóstico diferencial de outros tipos de demência e não existe um tratamento eficaz para essa
doença. Apresentamos neste artigo uma revisão da literatura baseada no relato de três casos da forma esporádica dessa doença.
Palavras-chave: Síndrome de Creutzfeldt-Jakob; Doenças Priônicas; Mioclonia.
INTRODUCTION CJD is classified into sporadic, variant,
C reutzfeldt-Jakob disease (CJD) was first
described in 1920 by Hans Gerhard
Creutzfeldt and Alfons Jakob1. It belongs
iatrogenic, and familial or genetic forms.
The sporadic form (sCJD) corresponds to
most cases, which do not have an infec-
to the group of transmissible spongiform tious source or evidence of familial dis-
encephalopathies (TSE), which are neurode- ease. The acquired forms are the variant
generative diseases caused by prions. CJD is CJD (vCJD), known as “mad cow disease,”
a rare disease, with an overall incidence of and the iatrogenic (iCJD), which is mainly
1–2 cases per million individuals each year. associated with dura mater graft and the
In Brazil, only 55 cases were confirmed use of human growth hormone 3,4. vCJD
between the years of 2005 and 2014 2 . was observed in 1980 in the UK popula-
The other human prion diseases are Kuru, tion after ingesting contaminated beef 5.
Gerstmann-Sträussler-Scheinker syndrome The familial CJD (fCJD) is defined as
(GSS), fatal familial insomnia (FFI), and vari- definite or probable CJD plus definite or
ably protease-sensitive prionopathy (VPSPr). probable CJD in a first-degree relative or
This study was conducted by the Santa Casa de Misericórdia de Sobral Hospital, Sobral, Ceará, Brazil.
1
Universidade Federal do Ceará, Faculdade de Medicina, Sobral CE, Brazil.
2
Santa Casa de Misericórdia de Sobral, Sobral CE, Brazil.
Correspondence: Amandha Alencar Maia Carneiro; Email: amandhacarneiro@yahoo.com.br.
Disclosure: The authors do not report conflicts of interest.
Funding: None.
Received on November 02, 2021; Received in its final form on February 15, 2022; Accepted on March 15, 2022.
Carneiro AAM, et al. Creutzfeldt-Jakob disease: literature review. 367
Views & Reviews
Dement Neuropsychol 2022 December;16(4):367-372
a disease-specific PrP gene mutation. About 10–15% and bodily myoclonus, when he was admitted to the hos-
of CJD cases are familial6. pital. The patient had no previous comorbidities and no
The sporadic form has a long incubation period, with family history of similar diseases. The CSF examination
an average age of onset of symptoms about 62 years and did not show alterations, and the immunoassay of the
survival of only 1 year after the onset of the condition. 14-3-3 protein in the CSF was negative. EEG showed
vCJD affects younger age group, with an average age of generalized periodic discharges with short periodicity,
onset of symptoms of 26 years, and has a longer dura- and the brain MRI showed hyperintensity in the head of
tion of about 14 months5,7. the caudate nucleus, lentiform nucleus, and diffuse cor-
As the patients with CJD develop rapidly progressive tical gyri, in addition to a cortical ribbon signal, on the
dementia, associated with myoclonus, visual or cerebel- T2-weighted, FLAIR, and DWI sequences. After 7 days
lar problems, pyramidal or extrapyramidal features, and of hospitalization, the patient died.
akinetic mutism, the hypothesis of CJD must be raised7.
Suggestive findings on brain magnetic resonance
imaging (MRI) and a positive result from a real-time CASE 3
quaking-induced conversion (RT-QuIC) support the A 47-year-old female, from Crateús-Ceará, in February
diagnosis. However, only brain tissue biopsy provides a 2021 started experiencing intense vertigo. In March
definitive diagnosis7. Other than clinical support, there of the same year, she presented ataxic gait, evolving a
is no treatment for this disease, which is uniformly fatal. month later with loss of ambulation, sensitive aphasia,
The purpose of this article is to review the literature myoclonus in the upper limbs, oral feeding movements,
based on the report of three cases of the sporadic form dullness, confabulations, hyperreligiosity, and halluci-
of CJD, which were diagnosed between 2018 and 2021, nations, when she was admitted to the hospital. The pa-
in the neurology service of the Santa Casa de Misericórdia tient presented hyperthyroidism as comorbidity, was
de Sobral hospital in Sobral, Ceará, Brazil. treated with tapazol, and revealed a history of first-de-
gree consanguinity between the parents. The analysis of
the CSF showed no alterations, with the immunoassay
CASE 1 of the 14-3-3 protein being negative. Brain MRI showed
A 69-year-old female, from Sobral-Ceará, in April 2017 a diffusion restriction signal in the putamen and caudate
started to experience progressive visual loss, headaches, nucleus bilaterally, associated with a cortical strand sig-
and vertigo. In October of the same year, she evolved nal in the frontal region, in the DWI, and T2-weighted
with ataxic gait, upper limb tremors, depressed mood, sequences. EEG showed periodic generalized bursts of
and short-term episodic memory deficit. In January biphasic and triphasic waves. During hospitalization,
2018, the patient was admitted to the hospital with the patient evolved with severe infectious complications
muscle stiffness, spasticity, myoclonus, and akinetic and atrial fibrillation. On the 39th day of hospitaliza-
mutism. There were no reports of similar illnesses in the tion, the patient died.
family. Brain MRI showed hyperintensity in the caudate
and lentiform nuclei bilaterally and in diffuse cortical
gyri on T2-weighted and FLAIR (fluid-attenuated in- DISCUSSION
version recovery) sequences and restricted diffusion CJD manifests itself in the presence of prions, which are
in the same regions in DWI/ADC (diffusion-weighted small particles containing an abnormal isoform (PrPSc)
imaging/apparent diffusion coefficient). The electroen- of a protein (PrPc) naturally present in the human body.
cephalogram (EEG) showed diffuse triphasic wave dis- The deposition of prions in brain tissue is responsible for
charges associated with periodic complexes with short neuronal dysfunction due to synaptic loss and cellular
periodicity. The immunoassay of the 14-3-3 protein in death, resulting in a spongiform appearance in tissue
the cerebrospinal fluid (CSF) was negative. The patient microscopy6,7. Prions are deposited in various regions
remained in palliative care and died in March 2018. of the body, but reach higher levels in the brain, retina,
and optic nerve, triggering the neurological and visual
symptoms of the disease5.
CASE 2 Demonstration of the transmissibility of CJD was
A 66-year-old male, from Irauçuba-Ceará, in March 2019 made in 1968, through the reproduction of the dis-
presented bradykinesia, ataxic gait, delusions, and at- ease and pathological findings in chimpanzees. It was
tempted suicide. In April of the same year, he developed observed that in prion diseases there is no detectable
torpor, right hemiparesis, spastic rigidity, and orofacial immunopathological response, the incubation period
368 Creutzfeldt-Jakob disease: literature review. Carneiro AAM, et al.
Views & Reviews
Dement Neuropsychol 2022 December;16(4):367-372
is prolonged, ranging from months to years, and the (Table 1). Evaluation of suspected cases includes brain
course of the disease is fatal, from weeks to months1,8. MRI, EEG, and analysis of CSF7. The cranial computed
The sporadic form of CJD has defined subtypes based tomography is usually normal, being useful, mainly, to
on focal neurological findings, which reflect the predom- exclude other conditions. The current diagnostic criteria
inant involvement of certain brain regions, e.g., predom- for CJD used in Europe are listed in Table 213. MRI is
inantly visual (Heidenhain variant), cerebellar (Oppen- an important mean of investigation in the sporadic
heimer-Brownell variant), cognitive, and affective forms9.
The main prodromes of CJD are anxiety, dizzi-
Table 2. Diagnostic criteria for surveillance of sporadic Creutzfeldt-Jakob
ness, blurred vision, asthenia, and unusual behavior8.
disease from January 1, 2017.
Such symptoms were present in the three cases report-
ed. The clinical picture of CJD is quite heterogeneous. 1.1 DEFINITE:
A very characteristic sign of the disease is myoclonus, Progressive neurological syndrome AND
often caused by varied sensory stimuli, which is present Neuropathologically or immunohistochemically or biochemically
confirmed
in 90% of cases8.
Neuropsychiatric symptoms include dementia, 1.2 PROBABLE:
behavioral and mood changes, such as apathy and 1.2.1: I + two of II and typical electroencephalogram*
depression, in addition to deficits in higher cortical OR 1.2.2: I + two of II and typical magnetic resonance imaging brain
scan+
functions, such as apraxia, aphasia, and visuospatial
OR 1.2.3: I + two of II and positive CSF 14-3-3
difficulties (e.g., spatial neglect, Balint’s syndrome)10. OR 1.2.4: Progressive neurological syndrome and positive real-time
Some patients may have psychotic symptoms, especially quaking-induced conversion in CSF or other tissues
visual hallucinations11, such as the patient mentioned
1.3 POSSIBLE:
in case 3. Cerebellar manifestations, such as nystag-
I + two of II + duration <2 years
mus and ataxia, occur in approximately two-thirds of
patients, and signs of involvement of the corticospinal I - Rapidly progressive cognitive impairment
tract, including hyperreflexia, Babinski’s sign, and II - A Myoclonus
spasticity, appear in 40–80% of cases. Some patients B Visual or cerebellar problems
may have extrapyramidal signs such as hypokinesia, C Pyramidal or extrapyramidal features
bradykinesia, dystonia, and rigidity. The final stage D Akinetic mutism
of the disease is characterized by akinetic mutism12. *Generalized periodic complexes; +high signal in caudate/putamen on magnetic resonance
All these symptoms are compatible with the clinical imaging brain scan or at least two cortical regions (temporal, parietal, occipital) on either
picture presented by patients in the three reported cases diffusion-weighted imaging or fluid-attenuated inversion recovery; CSF: cerebrospinal fluid.
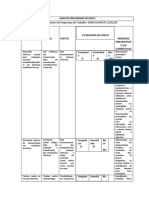
Table 1. Review of reported cases.
Case 1 Case 2 Case 3
Age 69 years 66 years 47 years
Time from symptom
12 months 3 months 5 months
onset to death
Hypokinesia, ataxic gait, psychosis,
Main signs and Vertigo, rigidity, ataxic gait, myoclonus, Vertigo, ataxic gait, sensory aphasia,
sensory aphasia, rigidity, and
symptoms and akinetic mutism myoclonus, and hallucinations
myoclonus
High signal in the head of the caudate
Diffusion restriction signal in putamen
High signal in caudate nucleus, nucleus, lentiform nucleus, and diffuse
and caudate nucleus, associated with
MRI findings lentiform, and diffuse cortical gyri on cortical gyri, in addition to “cortical
cortical ribbon signal in frontal region
DWI, T2-weighted, and FLAIR ribboning” signal on T2-weighted,
on DWI and T2-weighted
FLAIR, and DWI
Diffuse repetitive triphasic wave Diffuse repetitive wave discharges with Diffuse repetitive wave discharges with
EEG findings
discharges with short periodicity short periodicity short periodicity
Normal CSF Normal CSF Normal CSF
CSF findings
Negative 14-3-3 protein Negative 14-3-3 protein Negative 14-3-3 protein
MRI: magnetic resonance imaging; DWI: diffusion-weighted; FLAIR; fluid-attenuated inversion recovery; EEG: electroencephalogram; CSF: cerebrospinal fluid.
Carneiro AAM, et al. Creutzfeldt-Jakob disease: literature review. 369
Views & Reviews
Dement Neuropsychol 2022 December;16(4):367-372
form of CJD, as it is highly sensitive and specific, in findings may be present in other conditions, such as
addition to being widely available. The classic findings end-stage Alzheimer’s disease, Lewy body dementia,
of the disease are T2-FLAIR hyperintensity and re- and metabolic encephalopathies14. The three patients
stricted diffusion in the caudate, putamen and cortex, reported in this study presented these typical findings
which are present in 80% of cases14. The sensitivity and on brain MRI and EEG (Figure 1), associated with a com-
specificity of these findings are 83–92% and 87–95%, patible clinical picture, thus reinforcing the diagnosis of
respectively15. The typical EEG pattern shows bilateral CJD. CSF analysis is usually normal, although protein
synchronous periodic epileptiform discharges, such as levels may be elevated in 40% of patients8. Four proteins
biphasic or triphasic waves, with 90% specificity for have been detected by immunoassay or Western blot in
CJD, in a compatible clinical setting. However, these CSF, with high sensitivity for the detection of patients
Figure 1. Axial diffusion-weighted and fluid-attenuated inversion recovery images showing bilateral involvement of the basal ganglia (Cases 1 and 3 – white arrows)
and thalami (Case 1 – gray arrow). Axial diffusion-weighted shows more widespread signal hyperintensity in the cortical ribbon (Cases 2 and 3 – black arrows). Those
findings are reported as usual Creutzfeldt-Jakob disease magnetic resonance imaging signs. Regarding the electroencephalograms, it is possible to note a diffuse
repetitive triphasic wave discharges pattern with short periodicity in Case 1 and diffuse repetitive wave discharges pattern with short periodicity in Cases 2 and 3.
370 Creutzfeldt-Jakob disease: literature review. Carneiro AAM, et al.
Views & Reviews
Dement Neuropsychol 2022 December;16(4):367-372
with CJD: protein 14-3-3, tau, neuron-specific enolase, inoculated with prion protein, but no significant effects
and S-10016,17. A high level of non-phosphorylated were evidenced in clinical trials. Pentosan polysulfate
tau protein has greater specificity for the diagnosis of (PPS) is a high-molecular-weight polymer similar to
CJD when compared to 14-3-3 protein dosage. 14-3-3 heparin that appears to interfere with the conversion
protein dosage is considered an adjunct rather than a of PrPC to PrPSC when administered intraventricular-
diagnostic test, since its 80% of specificity applied to a ly. Studies have shown longer survival with the use of
disease with a prevalence as low as CJD means that most PPS, but there was a frequent association with subdu-
positive tests are actually false positives18. A negative ral hemorrhages, not being a viable treatment option.
test for this protein, as in the three cases reported, The association of quinacrine use with slower cognitive
does not exclude the diagnosis, as the sensitivity may decline in patients with sCJD remains controversial in
be lower in the early and late stages of the disease19,20. the clinical trials performed. Doxycycline was effective
However, the RT-QuIC test has made the diagnosis of in in vitro models and in animals with prion disease,
CJD easier, because it can detect minimal levels of prion possibly by preventing the abnormal folding of the pri-
protein in the CSF, increasing the chances of diagnosis on protein, but its clinical benefit remains uncertain22.
while still alive. The sensitivity and specificity of this Therefore, there is no effective treatment for CJD,
test are 91 and 98%, respectively21. which is uniformly fatal. Supportive measures include
It is important to note that MRI and EEG are easily symptomatic treatment of neuropsychiatric disorders
accessible tests, but the identification of the 14-3-3 pro- and myoclonus, which may respond satisfactorily to
tein and the RT-QuIC assay in CSF are still a challenge, benzodiazepines, such as clonazepam, and to certain
because they are not available in some hospitals in Brazil. anticonvulsants, such as levetiracetam and valproate23.
Considering the average age of onset of symptoms, CJD is a rare diagnosis that should be suspected in
it is possible that some cases of CJD are confused with cases of rapidly progressive dementia mainly associated
other neurological conditions that commonly affect with myoclonus. Typical findings on brain MRI and EEG
the elderly, such as Lewy body dementia, autoimmune support the diagnosis. However, new discoveries about
encephalitis, Alzheimer’s disease, and primary psychi- CJD are needed, including earlier diagnostic techniques
atric disorder5. and a treatment capable of modifying or delaying the
Over the past few years, some treatment possibilities fatal evolution of the disease.
for the sporadic form of CJD have been investigated, but
none of them have improved symptoms or increased Authors’ contributions. AAMC, MAE: writing – original
survival. Flupirtine, a centrally acting non-opioid anal- draft, writing – review & editing; DELS, EMLR: writing
gesic, showed cytoprotective activity in vitro in neurons – review & editing.
REFERENCES
1. Kouyoumdjian JA, Meneghette C, Tognola WA, Fonseca MG, Costa 9. Appleby BS, Appleby KK, Crain BJ, Onyike C, Wallin MT, Rabins PV. Cha-
RB. Creutzfeldt jakob disease: a case report. Arq Neuro-Psiquiatr. racteristics of established and proposed sporadic Creutzfeldt-Jakob di-
1987;45(1):53-9. https://doi.org/10.1590/S0004-282X1987000100007 sease variants. Arch Neurol. 2009;66(2):208-15. https://doi.org/10.1001/
2. Brazil – Ministério da Saúde. Creutzfeldt Jakob disease: causes, symptoms, archneurol.2008.533
diagnosis, treatment and prevention. 2019 [cited on July 26, 2021]. Available 10. Krasnianski A, Bohling GT, Heinemann U, Varges D, Meissner B, Schulz-S-
from: https://antigo.saude.gov.br/saude-de-a-z/doenca-de-creutzfeldt-jakob-dcj chaeffer WJ, et al. Neuropsychological symptoms in patients with sporadic
3. Svrcinova T, Manresa J, Mouchova Z, Kanovsky P. Creutzfeldt Jakob Creutzfeldt-Jakob disease in Germany. J Alzheimers Dis. 2017;59(1):329-
disease - a genetic form. J Neurol Sci. 2015;357:e113. https://doi. 37. https://doi.org/10.3233/JAD-161129
org/10.1016/j.jns.2015.08.361 11. Thompson A, MacKay A, Rudge P, Lukic A, Porter MC, Lowe J, et al.
4. Velásquez DC, Álzate AG, Lanau AV, Velásquez LME, Lopera JZ, Lopera Behavioral and psychiatric symptoms in prion disease. Am J Psychiatry.
F, et al. Human transmissible spongiform encephalopathy: case report.
2014;171(3):265. https://doi.org/10.1176/appi.ajp.2013.12111460
IATREIA 2014;27(3):330-6.
12. Rabinovici GD, Wang PN, Levin J, Cook L, Pravdin M, Davis J, et al.
5. Uttley L, Carroll C, Wong R, Hilton DA, Stevenson M. Creutzfeldt-Jakob di-
First symptom in Creutzfeldt-Jakob disease sporadic. Neurology
sease: a systematic review of global incidence, prevalence, infectivity, and
2006;66(2):286. https://doi.org/10.1212/01.wnl.0000196440.00297.67
incubation. Lancet Infect Dis. 2020;20(1):e2-e10. https://doi.org/10.1016/
s1473-3099(19)30615-2 13. National Creutzfeldt-Jakob Disease Research & Surveillance Unit. Uni-
6. Schelzke G, Kretzschmar HA, Zerr I. Clinical aspects of common genetic versity of Edinburgh. Protocol: surveillance of CJD in the UK [cited on
Creutzfeldt-Jakob disease. Eur J Epidemiol 2012;27(2):147-9. https://doi. April, 2017]. Available from: https://www.cjd.ed.ac.uk/sites/default/files/
org/10.1007/s10654-012-9660-3 NCJDRSU%20surveillance%20protocol-april%202017%20rev2.pdf.
7. Gallas LF, Morbeck DL, Queiroz AC. Human prion disease: correlation 14. Mackenzie G, Will R. Creutzfeldt-Jakob disease: recent developments
between clinical and pathological necropsy findings. Neuropsiquiatria F1000Research. 2017,6:2053. https://doi.org/10.12688/f1000resear-
2016, 20(1): 73-82. ch.12681.1
8. Jubelt B. Infectious diseases of the central nervous system. In: Rosenberg 15. Valente AP, Pinho PC, Lucato LT. Magnetic ressonance imaging in
RN, editor. Atlas of Clinical Neurology. 4th ed. Philadelphia: Springer, 2019. the diagnosis of Creutzfeldt-Jakob disease. Dement Neuropsychol.
p. 441-515. https://doi.org/10.1007/978-1-57340-359-7_12 2015;9(4):424-7. https://doi.org/10.1590/1980-57642015DN94000424
Carneiro AAM, et al. Creutzfeldt-Jakob disease: literature review. 371
Views & Reviews
Dement Neuropsychol 2022 December;16(4):367-372
16. Yun M, Wu W, Hood L, Harrington M. Human cerebrospinal fluid protein 20. Collins SJ, Sanchez-Juan P, Masters CL, Klug GM, Duijn CV, Poleggi
database-edition 1992. Electrophoresis. 1992;13(1):1002-13. https://doi. A, et al. Determinants of diagnostic investigation sensitivities across
org/10.1002/elps.11501301202 the clinical spectrum of sporadic Creutzfeldt-Jakob disease. Brain.
17. Blisard K, Davis L, Harrington M, Lovell JK, Kornfeld M, Berger ML. Pre- 2006;129(9):2278-87. https://doi.org/10.1093/brain/awl159
-mortem diagnosis of Creutzfeldt-Jakob disease by detection of abnormal 21. McGuire LI, Peden AH, Orrú CD, Wilham JM, Cbiol NEA, Mallinson G,
cerebrospinal fluid proteins. J Neurol Sci. 1990;99(1):75-81. https://doi. et al. Real time quaking-induced conversion analysis of cerebrospinal fluid
org/10.1016/0022-510x(90)90201-w
in sporadic Creutzfeldt-Jakob disease. Ann Neurol. 2012;72(2):278-85.
18. Hamlin C, Puoti G, Berri S, Sting E, Harris C, Cohen M, et al. A comparison
https://doi.org/10.1002/ana.23589
of tau and 14-3-3 protein in the diagnosis of Creutzfeldt-jakob disease. Neu-
rology. 2012;79(76):547. https://doi.org/10.1212/WNL.0b013e318263565f 22. Korth C, Peters PJ. Emerging pharmacotherapies for Creutzfeldt-Jakob
19. Muayqil T, Gronseth G, Camicioli R. Evidence-based guideline: diagnostic disease. Arch Neurol. 2006;63(4):497-501. https://doi.org/10.1001/
accuracy of CSF 14-3-3 protein in sporadic Creutzfeldt-Jakob disease: re- archneur.63.4.497
port of the guideline development subcommittee of the American Academy 23. Appleby BS, Yobs DR. Symptomatic treatment, care and support of
of Neurology. Neurology. 2012;79(14):1499. https://doi.org/10.1212/ patients with CJD. Handb Clin Neurol. 2018;153:399-408. https://doi.
WNL.0b013e31826d5fc3 org/10.1016/B978-0-444-63945-5.00021-0
372 Creutzfeldt-Jakob disease: literature review. Carneiro AAM, et al.
Você também pode gostar
- Revisão literária da doença de Alzheimer: o impacto no âmbito familiarNo EverandRevisão literária da doença de Alzheimer: o impacto no âmbito familiarAinda não há avaliações
- Doença de Creutzfeldt-Jakob Relato de Caso. Rev Soc Bras 2019Documento4 páginasDoença de Creutzfeldt-Jakob Relato de Caso. Rev Soc Bras 2019Mariano David Díaz GambiniAinda não há avaliações
- DOENÇA DE CREUTZFELDT-JAKOB. Casos Notificados e Confirmados No Estado de Minas. 2017Documento8 páginasDOENÇA DE CREUTZFELDT-JAKOB. Casos Notificados e Confirmados No Estado de Minas. 2017Mariano David Díaz GambiniAinda não há avaliações
- Doenças Priônicas e A VigilânciaDocumento47 páginasDoenças Priônicas e A VigilânciaSoraia Nogueira FelixAinda não há avaliações
- Relato de Caso Sindrome de Phelan-McdermidDocumento4 páginasRelato de Caso Sindrome de Phelan-McdermidElison e Juliana CavassinAinda não há avaliações
- Boletim Epidemiológico Vol.53 Nº39Documento12 páginasBoletim Epidemiológico Vol.53 Nº39GrennAinda não há avaliações
- Doena de Creutzfeldt-Jakob (DCJ)Documento21 páginasDoena de Creutzfeldt-Jakob (DCJ)João BoscoAinda não há avaliações
- Cognitive Dysfunction in Corticobasal DegenerationDocumento10 páginasCognitive Dysfunction in Corticobasal Degenerationerika avelina rodriguez jaureguiAinda não há avaliações
- Eduardo, Demência de Corpos de LewyDocumento13 páginasEduardo, Demência de Corpos de LewyFlavioAinda não há avaliações
- Doença de Creutzfeldt-Jakob (DCJ) - Português (Brasil)Documento5 páginasDoença de Creutzfeldt-Jakob (DCJ) - Português (Brasil)Ivan Ferreira de AraujoAinda não há avaliações
- Dabaly. Medicina GeralDocumento11 páginasDabaly. Medicina GeralJanuário Virgílio DabaliAinda não há avaliações
- Bioq Apre G7Documento16 páginasBioq Apre G7deividAinda não há avaliações
- 1 PBDocumento10 páginas1 PBLarissa AcraniAinda não há avaliações
- N2 - FinalizadoDocumento6 páginasN2 - FinalizadoPamela SouzaAinda não há avaliações
- 189716-Texto Do Artigo-565274-1-10-20220706Documento7 páginas189716-Texto Do Artigo-565274-1-10-20220706João Manoel Sousa SoaresAinda não há avaliações
- Sindrome de DigeorgeDocumento4 páginasSindrome de DigeorgeIsis MariaAinda não há avaliações
- 6331-Manuscrito Original-27603-1-10-20160719Documento11 páginas6331-Manuscrito Original-27603-1-10-20160719Jéssica LimaAinda não há avaliações
- A Linha Ténue Entre A Demência e Depressão No IdosoDocumento7 páginasA Linha Ténue Entre A Demência e Depressão No IdosoMiguel PlenoAinda não há avaliações
- Sindrome CADASILDocumento33 páginasSindrome CADASILEduardo NolascoAinda não há avaliações
- 160-Texto Do Artigo-276-285-10-20210629Documento4 páginas160-Texto Do Artigo-276-285-10-20210629Musashi GutsAinda não há avaliações
- Apresentação Clínica Da Doença de Creutzfeldt MinutaDocumento2 páginasApresentação Clínica Da Doença de Creutzfeldt MinutaDiego CorreiaAinda não há avaliações
- Avaliação de Genética Clínica 2021.2Documento5 páginasAvaliação de Genética Clínica 2021.2José Ribeiro NetoAinda não há avaliações
- Seminário Biologia Doenças PriônicasDocumento10 páginasSeminário Biologia Doenças Priônicaselasantos0905Ainda não há avaliações
- Baptista 2017 Case ReportDocumento4 páginasBaptista 2017 Case ReportNatammyAinda não há avaliações
- ResumosDocumento61 páginasResumosRoger piresAinda não há avaliações
- Intervencoes Do Enfermeiro A Pessoa Com Doenca de AlzheimerDocumento13 páginasIntervencoes Do Enfermeiro A Pessoa Com Doenca de AlzheimerClarinhaAinda não há avaliações
- Paralisia Do Nervo Oculomotor Como Manifestação Inicial de Esclerose Múltipla Relato de CasoDocumento7 páginasParalisia Do Nervo Oculomotor Como Manifestação Inicial de Esclerose Múltipla Relato de CasomarianabrantnobreAinda não há avaliações
- Artigo Epilepsia - Lann - SictegDocumento1 páginaArtigo Epilepsia - Lann - SictegJose Victor Lima de SouzaAinda não há avaliações
- 1 PBDocumento8 páginas1 PBGabriela Mendes da SilvaAinda não há avaliações
- Ataxia de Friedreich - Análise de EstudosDocumento10 páginasAtaxia de Friedreich - Análise de EstudosYuzo IgarashiAinda não há avaliações
- Non-Inflammatory Cerebral Amyloid Angiopathy As A Cause of Rapidly Progressive DementiaDocumento6 páginasNon-Inflammatory Cerebral Amyloid Angiopathy As A Cause of Rapidly Progressive Dementiayalocim666Ainda não há avaliações
- Trombose Venosa Cerebral: Estudo de Sete Casos: Cerebral Venous Thrombosis: Study of Seven CasesDocumento7 páginasTrombose Venosa Cerebral: Estudo de Sete Casos: Cerebral Venous Thrombosis: Study of Seven Caseselisson.blimaAinda não há avaliações
- Esclerose MúltiplaDocumento7 páginasEsclerose Múltiplaspilingueta_71394279Ainda não há avaliações
- 1 s2.0 S1413867022002227 MainDocumento2 páginas1 s2.0 S1413867022002227 Maingeovaninha.oliveiraAinda não há avaliações
- Doenças Psiquiátricas e o Sistema CardiovascularDocumento11 páginasDoenças Psiquiátricas e o Sistema CardiovascularGe NomAinda não há avaliações
- Características Clínicas e Epidemiológicas de 20 Pacientes Portadores de Esclerose Múltipla Acompanhados em CuiabáDocumento4 páginasCaracterísticas Clínicas e Epidemiológicas de 20 Pacientes Portadores de Esclerose Múltipla Acompanhados em CuiabáHiroki ShinkaiAinda não há avaliações
- Distrofia Musculatr de UlrichDocumento4 páginasDistrofia Musculatr de UlrichLeonardo06041991Ainda não há avaliações
- Avaliação Neuropsicológica Na Doença de Alzheimer E No Comprometimento Cognitivo LeveDocumento11 páginasAvaliação Neuropsicológica Na Doença de Alzheimer E No Comprometimento Cognitivo LeveThaíssa Ágatha BaraunaAinda não há avaliações
- 3 - Crise Convulsiva FebrilDocumento4 páginas3 - Crise Convulsiva FebrilClara Liz Pinto PedrosaAinda não há avaliações
- "Principais Grupos Populacionais" - Fenótipo e Genótipo Da Deficiencia IntelectualDocumento14 páginas"Principais Grupos Populacionais" - Fenótipo e Genótipo Da Deficiencia IntelectualvanessaAinda não há avaliações
- Artigo CCL e DADocumento10 páginasArtigo CCL e DAMaria Victoria Ruperti ZimmermannAinda não há avaliações
- Alzheimer-1-19 PTDocumento35 páginasAlzheimer-1-19 PTJessé AraújoAinda não há avaliações
- 2253-Texto Do Artigo-8923-1-10-20170224Documento10 páginas2253-Texto Do Artigo-8923-1-10-20170224Marcelo GuimaraesAinda não há avaliações
- 5898-Texto Do Artigo - Arquivo Original-27568-1-10-20180212Documento11 páginas5898-Texto Do Artigo - Arquivo Original-27568-1-10-20180212Instituto Integrado em PsicologiaAinda não há avaliações
- Estudo LongitudinalDocumento6 páginasEstudo LongitudinaldenikkjohnAinda não há avaliações
- Síndrome Do PirilampoDocumento6 páginasSíndrome Do PirilampoBruce MarlonAinda não há avaliações
- Trabalho de Investigação de BioDocumento14 páginasTrabalho de Investigação de BioRaissa AndreattiAinda não há avaliações
- 33591-Manuscrito No Template Padrão RBE-124512-4!10!20191205Documento9 páginas33591-Manuscrito No Template Padrão RBE-124512-4!10!20191205LucasFreitasChavesAinda não há avaliações
- Toxoplasmosis Cerebral yDocumento8 páginasToxoplasmosis Cerebral yMIGUEL GALEANO AndradesAinda não há avaliações
- DMy AlzheimerDocumento9 páginasDMy AlzheimerJUAN DIEGO TUCTO HERNÁNDEZAinda não há avaliações
- Caso ClinicoDocumento3 páginasCaso ClinicoausendanunesAinda não há avaliações
- 24214c DC Distrofia Muscular de DuchenneDocumento10 páginas24214c DC Distrofia Muscular de DuchenneMariele Faccin MontagnerAinda não há avaliações
- Down Syndrome in Adults Success and ChallengeDocumento7 páginasDown Syndrome in Adults Success and ChallengewalkersvillemomAinda não há avaliações
- Distrofia Muscular de Becker.Documento6 páginasDistrofia Muscular de Becker.underklowAinda não há avaliações
- Assistência de Enfermagem Aos Pacientes Portadores de Alzheimer Uma Revisão Integrativa LILACSDocumento4 páginasAssistência de Enfermagem Aos Pacientes Portadores de Alzheimer Uma Revisão Integrativa LILACSJosi LimaAinda não há avaliações
- Apresentação 1Documento34 páginasApresentação 1Osvaldo InácioAinda não há avaliações
- Doença de Menkes: Relato de Caso: Menkes' Disease: Case ReportDocumento5 páginasDoença de Menkes: Relato de Caso: Menkes' Disease: Case ReportSem nomeAinda não há avaliações
- Problema 08Documento3 páginasProblema 08Gabriel SebaAinda não há avaliações
- Atraso Do Desenvolvimento PsicomotorDocumento6 páginasAtraso Do Desenvolvimento PsicomotorPetraAlexandraAinda não há avaliações
- DepressãoDocumento13 páginasDepressãoTranpsAinda não há avaliações
- Saúde Do Homem NovoDocumento18 páginasSaúde Do Homem NovoAlfa Filho100% (2)
- Acfrogbhkxk9qcoggqdsjyyii3f727pxrgayshjxfjuwlim Zcd89 Ppmrius Bmp5ok Zyzxo2bqslxet1y C2gfafjr4bh98sww1ezr1tcslc Yeiwa5fimhotx5ijzgsnqnu Ksigx PecruDocumento70 páginasAcfrogbhkxk9qcoggqdsjyyii3f727pxrgayshjxfjuwlim Zcd89 Ppmrius Bmp5ok Zyzxo2bqslxet1y C2gfafjr4bh98sww1ezr1tcslc Yeiwa5fimhotx5ijzgsnqnu Ksigx PecruJúlio CésarAinda não há avaliações
- Aula 3. Critérios de Admissão e Alta em UTIDocumento24 páginasAula 3. Critérios de Admissão e Alta em UTILeticia Costa75% (4)
- Tombamento de Mudas - PáginaDocumento6 páginasTombamento de Mudas - PáginaCaciara Gonzatto MacielAinda não há avaliações
- ALTERAÇÕES CAPILARES e TRATAMENTOSDocumento44 páginasALTERAÇÕES CAPILARES e TRATAMENTOSTHATYANE SIMÃOAinda não há avaliações
- Terapia Nutricional Na Fibrose Cistica PDFDocumento9 páginasTerapia Nutricional Na Fibrose Cistica PDFAndreia Oliveira ChahhoudAinda não há avaliações
- Doenca de Von GierkeDocumento27 páginasDoenca de Von GierkeNathana VenancioAinda não há avaliações
- Nuflex 3Documento9 páginasNuflex 3Otavio MeloAinda não há avaliações
- Hérnia de HiatoDocumento8 páginasHérnia de HiatoRodrigo Morais Ribeiro de SantanaAinda não há avaliações
- Redução Dia de Sorte-21 Dzs Até14 dzs-99 % (7 PONTOS) #2Documento4 páginasRedução Dia de Sorte-21 Dzs Até14 dzs-99 % (7 PONTOS) #2naldoalexAinda não há avaliações
- SA 5 Rotinas de Saude e SegurançaDocumento9 páginasSA 5 Rotinas de Saude e SegurançaEster Aline Puschmann100% (2)
- Reta Final Fhemig 120 Questoes FGVDocumento105 páginasReta Final Fhemig 120 Questoes FGVKond GamesAinda não há avaliações
- Aula - Ornito - Influenza AviariaDocumento8 páginasAula - Ornito - Influenza AviariaIris MendesAinda não há avaliações
- Diarreia AgudaDocumento13 páginasDiarreia AgudaJuliana OliveiraAinda não há avaliações
- Biologia 3 AnoDocumento27 páginasBiologia 3 AnoRubens OliveiraAinda não há avaliações
- Resumo GO - IntegradaDocumento32 páginasResumo GO - IntegradaISABELA MENDES RODRIGUESAinda não há avaliações
- Regulamento CBV 2023 Abonação e Termo ResponsabilidadeDocumento3 páginasRegulamento CBV 2023 Abonação e Termo ResponsabilidadeAna Luisa AraujoAinda não há avaliações
- Article 297119 1 10 20220117Documento9 páginasArticle 297119 1 10 20220117Gisele CanelaAinda não há avaliações
- INJETAVEIS MED 2019abrilDocumento115 páginasINJETAVEIS MED 2019abrilAdriano BorgesAinda não há avaliações
- 2014 Prova XV TEAC CorrgidoDocumento36 páginas2014 Prova XV TEAC CorrgidoPaulo Henrique MaiAinda não há avaliações
- Descubra Como Escolher Um Plano de Saúde para Seu PetDocumento6 páginasDescubra Como Escolher Um Plano de Saúde para Seu PetPromoções PetAinda não há avaliações
- APENDICITEDocumento76 páginasAPENDICITEGeorge ViníciusAinda não há avaliações
- Management and Prognosis of The Zollinger-Ellison Syndrome (Gastrinoma) - UpToDateDocumento12 páginasManagement and Prognosis of The Zollinger-Ellison Syndrome (Gastrinoma) - UpToDateLarissa MeloAinda não há avaliações
- Semana Da Aprovacao Susba - GoDocumento46 páginasSemana Da Aprovacao Susba - GoFilipe AlbanAinda não há avaliações
- Cofen - Conselho Federal de Enfermagem RESOLUÇÃO COFEN #688 - 2022 - ALTERADA PELA RESOLUÇÃO COFEN #718 - 2023 PrintDocumento8 páginasCofen - Conselho Federal de Enfermagem RESOLUÇÃO COFEN #688 - 2022 - ALTERADA PELA RESOLUÇÃO COFEN #718 - 2023 PrintEduardo Fernando SouzaAinda não há avaliações
- Rev Valores Referencia Ingestao Nutrientes CriancasDocumento10 páginasRev Valores Referencia Ingestao Nutrientes CriancasCamila QueirozAinda não há avaliações
- Doenças Linfáticas PDFDocumento24 páginasDoenças Linfáticas PDFcrisAinda não há avaliações
- Farmacologia Da TireoideDocumento5 páginasFarmacologia Da TireoideHeloisa SantosAinda não há avaliações
- Livro HomeopatiaDocumento327 páginasLivro HomeopatiaCarina Anchieta100% (3)
- Congestão e EdemaDocumento4 páginasCongestão e EdemaRenata MendesAinda não há avaliações
- Treinamento cerebral: Compreendendo inteligência emocional, atenção e muito maisNo EverandTreinamento cerebral: Compreendendo inteligência emocional, atenção e muito maisNota: 4.5 de 5 estrelas4.5/5 (169)
- Biomecânica Básica dos Exercícios: Membros InferioresNo EverandBiomecânica Básica dos Exercícios: Membros InferioresNota: 3.5 de 5 estrelas3.5/5 (8)
- Detox de 10 dias: Como os sucos verdes limpam o seu organismo e emagrecemNo EverandDetox de 10 dias: Como os sucos verdes limpam o seu organismo e emagrecemNota: 2 de 5 estrelas2/5 (1)
- O fim da ansiedade: O segredo bíblico para livrar-se das preocupaçõesNo EverandO fim da ansiedade: O segredo bíblico para livrar-se das preocupaçõesNota: 5 de 5 estrelas5/5 (16)
- Desbloqueie o poder da sua mente: Programe o seu subconsciente para se libertar das dores e inseguranças e transforme a sua vidaNo EverandDesbloqueie o poder da sua mente: Programe o seu subconsciente para se libertar das dores e inseguranças e transforme a sua vidaNota: 4.5 de 5 estrelas4.5/5 (226)
- 21 dias para curar sua vida: Amando a si mesmo trabalhando com o espelhoNo Everand21 dias para curar sua vida: Amando a si mesmo trabalhando com o espelhoNota: 4.5 de 5 estrelas4.5/5 (49)
- TDAH em Adultos - Como Reconhecer e Lidar Com Adultos Que Sofrem de TDAH Em 30 Passos SimplesNo EverandTDAH em Adultos - Como Reconhecer e Lidar Com Adultos Que Sofrem de TDAH Em 30 Passos SimplesNota: 4.5 de 5 estrelas4.5/5 (8)
- Encantamentos, Rezas E BenzedurasNo EverandEncantamentos, Rezas E BenzedurasNota: 4.5 de 5 estrelas4.5/5 (10)
- Emoções: Introdução à psicologia das emoções. De Darwin à neurociência, o que são as emoções e como elas funcionamNo EverandEmoções: Introdução à psicologia das emoções. De Darwin à neurociência, o que são as emoções e como elas funcionamNota: 5 de 5 estrelas5/5 (4)
- A Cosmética das Ervas - Chás Capilares: Utilizando o poder das ervas para a saúde dos cabelosNo EverandA Cosmética das Ervas - Chás Capilares: Utilizando o poder das ervas para a saúde dos cabelosNota: 4.5 de 5 estrelas4.5/5 (2)
- Reflexoterapia: Corpo integrado- saúde totalNo EverandReflexoterapia: Corpo integrado- saúde totalNota: 3.5 de 5 estrelas3.5/5 (5)
- E-TRAP: entrevista diagnóstica para transtornos de personalidadeNo EverandE-TRAP: entrevista diagnóstica para transtornos de personalidadeNota: 5 de 5 estrelas5/5 (3)
- Psicoterapia breve: Abordagem sistematizada de situações de criseNo EverandPsicoterapia breve: Abordagem sistematizada de situações de criseNota: 4.5 de 5 estrelas4.5/5 (8)
- Hackeando Darwin: Engenharia genética e o futuro da humanidadeNo EverandHackeando Darwin: Engenharia genética e o futuro da humanidadeAinda não há avaliações